Baby Formula Buying Guide

Baby & Health Writer
Feeding a baby generally comes with a steep learning curve, no matter if it’s your first or your fourth, and regardless of the feeding method you choose. That’s because every baby is different—even siblings within the same family—and what works well for one child may not work for another.
The same applies when it comes to choosing the best infant formula. There are plenty of good options out there, but the best formula for your baby will be one they tolerate well, is safe, fits your budget, and is readily available.
Staring down the baby formula aisle can be overwhelming, to say the least. Understanding infant formula safety regulations and ingredient labels can be tricky (especially when you’re running on little sleep). Here’s what to know about choosing an infant formula that you can feel good about feeding to your baby.
- Where to Start When Choosing an Infant Formula
- What’s in Baby Formula?
- Types of Baby Formula
- How to Read a Baby Formula Label
- How to Choose a Baby Formula
- What to Know About Baby Formula Safety Regulations and Recalls
- What to Know About European Baby Formulas
- Best Practices for Formula Feeding
- Tips for Transitioning to Formula From Breast Milk
- How to Switch Formulas
- What to Know About Toddler Formulas
- FAQs About Formula Feeding
- Baby Formula Brands
Where to Start When Choosing an Infant Formula
While the American Academy of Pediatrics (AAP) encourages breastfeeding (exclusively for the first 6 months, and then alongside solid foods through 2 years of age and beyond as desired), not all infants are exclusively breastfed for a wide variety of reasons. It’s estimated that 60 percent of infants are not breastfeeding at all at 1 year of age. In those cases, AAP recommends using an iron-fortified infant formula as the best and safest alternative to breast milk in a baby’s first year.
Here’s the thing about choosing a baby formula: Thanks to strict nutrition regulations, any formula sold in the U.S. must contain all the essential nutrients your baby needs in their first year to help them grow. The biggest differences between formulas tend to be found in the types of proteins, carbohydrates, and fats they contain, plus any additional ingredients included to mimic breast milk or support your baby’s healthy development.
Your pediatrician is your best bet for specific formula recommendations based on your baby’s unique needs. Many parents start formula-feeding with a cow’s milk-based infant formula, the most widely available and cost-conscious option (goat milk- and soy-based formulas are often more expensive). Some families may consider switching to a different protein source if their infant seems to be having trouble digesting their current formula—more on those signs and symptoms below—though most babies tolerate cow milk-based formulas just fine.
If your baby is under 2 months of age, was born prematurely, or is immunocompromised, the Food and Drug Administration recommends starting with a ready-to-feed variety that doesn’t require adding water. After two months, you can probably switch to powdered formula, which tends to be more budget-friendly. Below, we’ll do a deep dive into the details behind these recommendations, along with a general overview of the formula options available.
What’s in Baby Formula?
Baby formula is designed to mimic breast milk and serve as an infant’s first food, either alongside or in place of breastfeeding. Infant formula is primarily made of macronutrients (carbohydrates, protein, and fat) and micronutrients (vitamins and minerals). It may also contain some components found in breast milk, like prebiotics, probiotics, and nucleotides (more on these below).
While formula ingredients can differ across brands, it’s important to know that all infant formulas sold in the U.S. must meet strict nutritional requirements outlined by the FDA. These guidelines are designed to ensure that all formulas sold in the U.S. provide the necessary protein, fats, carbohydrates, vitamins, and minerals a healthy, full-term infant needs from birth through 12 months, with the addition of solid food starting around 6 months.
Macronutrients in Baby Formula
As an infant’s potential sole food source, all baby formulas must contain the three macronutrients: carbohydrates, fats, and proteins. These are sources of calories your baby’s growing body needs, and make up the bulk of formula contents—in fact, at least 98 percent of what’s in the can are macronutrients. But the sources and amounts of those nutrients can differ. You might see the following on the formula label:
Carbohydrates:
• Lactose (the source of carbohydrates in breast milk)
• Corn syrup or corn syrup solids
• Maltodextrin
• Glucose
• Sucrose
• Rice starch (used as a thickener)
Proteins:
• Milk protein isolate
• Whey protein (concentrate or isolate)
• Soy protein isolate
• Casein hydrolysate
Fats:
• High oleic oil (usually safflower or sunflower oil)
• Palm oil or palm olein
• Soybean oil
• Coconut oil
• Canola or rapeseed oil
Which form of carbs, fats, and proteins you choose in your baby’s formula is up to you and your child’s pediatrician. Here’s what can help guide your decision.
A Note on Carbohydrates
Most experts recommend starting with an infant formula that lists lactose as the first ingredient, which is most similar to breast milk. It’s a common misconception that babies can’t digest lactose—most infants are born with the ability to digest this type of milk sugar.
“Lactose intolerance in adults is common, but incredibly rare in infants,” says Bridget E. Young, PhD, an associate professor of pediatrics at the University of Rochester School of Medicine and Dentistry, and the founder of babyformulaexpert.com. “Drinking lactose as a baby is part of what makes us mammals!”
Some infants, however, are allergic to the proteins in cow’s milk-based infant formulas, known as cow’s milk protein allergy (CMPA). Your child’s doctor can help you spot the signs, which may include excessive crying and fussiness, poor feeding, eczema, loose or watery stools, blood in stool, and in rare cases, anaphylaxis. If your child is diagnosed with CMPA, their healthcare provider may recommend a fully hydrolyzed formula to help with digestion: more on this in the “Extensively Hydrolyzed Infant Formula” and “Specialized Infant Formula” sections below.
In place of lactose, some formulas use corn syrup or corn syrup solids as a primary source of carbohydrates, for several reasons:
• It’s inexpensive to produce, which can help keep formula costs down.
• It’s easy to digest for infants who have still-developing digestive systems.
• It’s an alternative to lactose for those who may have conditions or allergies that prevent them from consuming breast milk or other types of formula.
• It’s a very sweet sugar, and is typically used in formulas with broken-down (hydrolyzed) proteins, which may help mask the bitter taste.
It’s worth noting that corn syrup and corn syrup solids are not the same as high-fructose corn syrup (HFCS), which has undergone further processing to increase the amount of fructose. No U.S. formulas currently contain HFCS.
While corn syrup’s use in infant formula has been shown to support infants’ growth, recent observational research shows that babies fed formula made with corn syrup may have a higher risk of obesity in the first five years of life. But this doesn’t mean there’s a direct link: More research is needed, and numerous factors can contribute to a person’s weight and health status beyond diet, such as genetics, environment, socioeconomic status, access to healthcare, and other social determinants of health. Though corn syrup and corn syrup solids in formula are banned in the E.U., the FDA does not set limits on corn syrup’s use in formula, and it can be hard to avoid: some hydrolyzed formulas use corn syrup as their primary carbohydrate source, rather than lactose.
A Note on Proteins
The three approved protein sources for infant formula are cow, goat, or soy milk. Some animal milk-derived formulas start with a whole, skim, or nonfat milk base and then add additional protein, often listed as a “protein isolate.”
To mimic breast milk’s composition more closely, many formula manufacturers add extra whey protein. While cow’s milk naturally contains about 20 percent whey and 80 percent casein, human milk has a higher whey content—approximately 60 percent whey and 40 percent casein. When you see whey protein on the ingredients list, it typically indicates that the formula has been adjusted to more closely match the whey-to-casein ratio of breast milk, which may support easier digestion for infants.
Soy-based formulas may be recommended for babies with allergies to animal milk proteins, but speak with your doctor about whether it’s the right choice for your little one.
A Note on Fats
Infant formulas commonly include plant-based fats—either on their own or alongside whole cow’s milk or goat milk, which provide animal-derived fats. Plant-based sources typically include seed oils such as sunflower, safflower, rapeseed, and soybean, and fruit oils like palm and coconut.
Whether from seeds, palm, or coconut, these fats have been shown to support babies’ healthy growth and development when included in formula. They provide essential fatty acids that are vital for cell function, immune regulation, brain development, and metabolism.
Seeds are processed into oil in several ways. Some formula manufacturers use an expeller-pressed method, but most seed oils are extracted using a chemical solvent called hexane, which is later removed. Both processes are generally considered safe.
Some research shows that babies who consume infant formula with a primary fat source of palm olein oil may absorb less fat and calcium than babies consuming formula without palm olein oil. This may be something to keep in mind when choosing a formula, especially for premature babies who have higher vitamin and mineral needs for growth and development.
Your pediatrician or family doctor can help you choose the best combination of carbohydrates, protein, and fats for your baby’s needs, and can help answer questions about different formula ingredients.
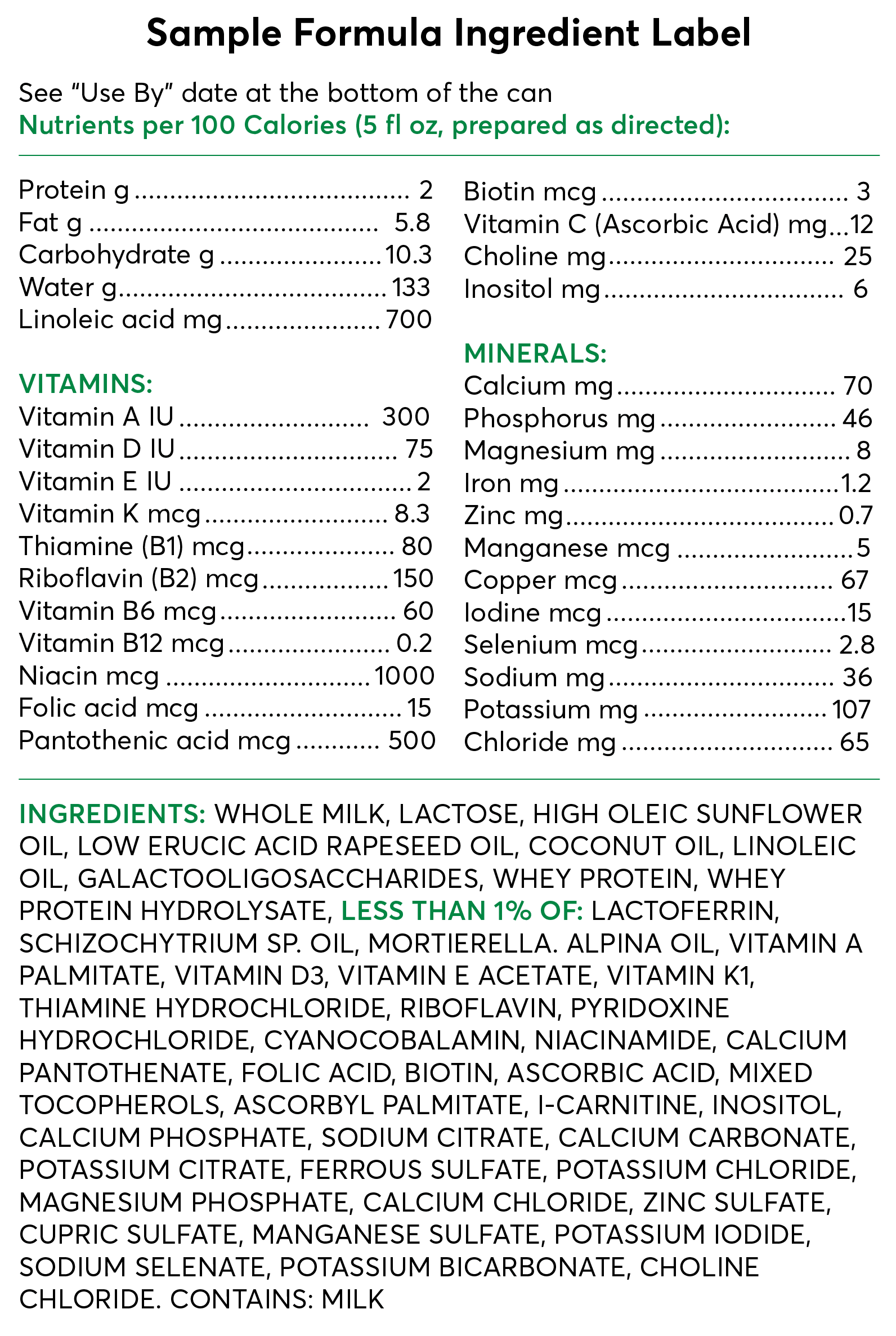
Wondering how these nutrients might appear on the infant formula label? See: “Decoding an Infant Formula Ingredient List,” below.
Micronutrients in Baby Formula
The FDA stipulates that infant formulas must include 27 different types of vitamins and minerals, known as micronutrients, at levels essential for babies’ health and growth in the first year. See the full list under "Decoding an Infant Formula Ingredients List,” below.
Cow’s milk, which is used as a base for many infant formulas, contains some naturally occurring micronutrients, like vitamin A, vitamin B12, calcium, and phosphorus, among others, but formula companies may include additional vitamins and minerals to meet the minimum levels required by the FDA, without exceeding the maximum levels set for 10 of those nutrients.
You can rest assured that any formula authorized for sale in the U.S. will contain at least the baseline amounts of vitamins and minerals your baby needs for development—unless you’re using a low-iron formula, in which case, you should talk to your child’s pediatrician about supplementing with additional iron.
Additional Ingredients in Baby Formula
You might see specific additional components called out on baby formula labels, like DHA, prebiotics, probiotics, nucleotides, and other “non-nutrients.” But are they truly necessary for babies’ growth and development?
“Additional nonrequired ingredients are precisely that: not required,” says Young. “All these ‘sexy extra’ ingredients are approved for safety in the formula, which is always our first concern.” They’re also all based on what’s found in breast milk. “If your baby is getting any amount of breast milk, they’re already getting all of these ingredients, and in a form that is likely to be more bioavailable" (better able to be absorbed and used by the body), Young says.
She also points out that while these extra ingredients make up just a tiny fraction of the formula (usually less than 2 percent), they are the subject of most of the marketing. “Research suggests that this marketing is often poorly substantiated and unreferenced,” says Young, so don’t put too much stock in the claims on the container.
Here’s what some of those extra ingredients are designed to do.
Extra ingredient: Docosahexaenoic acid (DHA) and arachidonic acid (ARA)
How it appears on the label: Crypthecodinium cohnii oil, Mortierella alpina oil, Schizochytrium sp. oil, DHA algal oil, tuna fish oil
What it does: These long-chain polyunsaturated fatty acids tend to accumulate in infants’ eyes and brains in the last trimester of pregnancy and are also found in breast milk.
Why it’s there: Studies are mixed on DHA/ARA, with some showing a benefit in visual function and cognitive development, including attention, processing, and learning, and others showing no real effect. But Young shares that DHA and ARA are currently included in every available U.S. formula.
Extra ingredient: Lutein
How it appears on the label: Lutein
What it does: A carotenoid (pigment that gives color to plants) with antioxidant properties, supporting the development of infant brain regions important for learning and visual processing
Why it’s there: Breast milk contains lutein, and one clinical trial of formula fortified with lutein shows it to be safe, but more research is needed to support its benefits in infant formula.
Extra ingredient: Milk fat globule membrane (MFGM)
How it appears on the label: Whey protein concentrate. Note that this ingredient also naturally occurs in whole cow’s milk or whole goat milk and may not always be added separately.
What it does: MFGM is a layer that surrounds fat droplets in all mammal milk, protecting them through digestion.
Why it’s there: Studies show some benefits for infant brain development and its use as an emulsifier in formula. But there’s still much we don’t know about how MFGM works.
Extra ingredient: Lactoferrin
How it appears on the label: Lactoferrin
What it does: This protein is found in both colostrum and breast milk and is absorbed into the bloodstream intact. It may have antimicrobial properties.
Why it’s there: Research shows it may help reduce infection in infants,, but studies of its use in formula are limited. One study showed babies fed formula with lactoferrin have soft stools similar to breastfed babies, but the formula also contained prebiotics.
Extra ingredient: Alpha-lactalbumin (alpha-lac)
How it appears on the label: Alpha-lactalbumin whey protein
What it does: A complete protein, it serves as a source of essential amino acids. It’s one of the most abundant whey proteins in breast milk and is also found in cow’s milk.
Why it’s there: Mainly to mimic the protein profile of breast milk. Studies have looked at safety, growth, and tolerance of formulas with added alpha-lac, but not specific benefits.
Extra ingredient: Nucleotides
How it appears on the label: Cytidine 5′-monophosphate, uridine 5′-monophosphate, and adenosine 5′-monophosphate, guanosine 5′-monophosphate, and inosine 5′-monophosphate
What it does: These nucleotides serve as precursors to nucleic acids, which are the building blocks for DNA and RNA (human genetic material).
Why it’s there: One study showed that formula with nucleotides contributed to infant growth and weight gain. It may also support immune function and digestion.
Extra ingredient: Prebiotics
How it appears on the label: Galactooligosaccharides (GOS), 2’-Fucosyllactose (2’-FL), fructo-oligosaccharides (FOS), polydextrose
What it does: It serves as food for gut bacteria and can help develop the infant gut microbiome.
Why it’s there: 2’-FL is a type of human milk oligosaccharide, or chain of sugar molecules, that has been shown to benefit infants, including by lowering risk of illness. But for GOS, polydextrose, and FOS, a systematic review found no significant benefit.
Extra ingredient: Probiotics
How it appears on the label: Lactobacillus reuteri, Bifidobacterium lactis, Bifidobacterium breve M-16V
What it does: These beneficial bacteria may colonize an infant’s digestive tract.
Why it’s there: Studies have shown some benefits of adding probiotics to formula, such as fewer infections, fewer episodes of diarrhea, and possibly a lower risk of eczema in babies, though more research is needed.
Types of Baby Formula
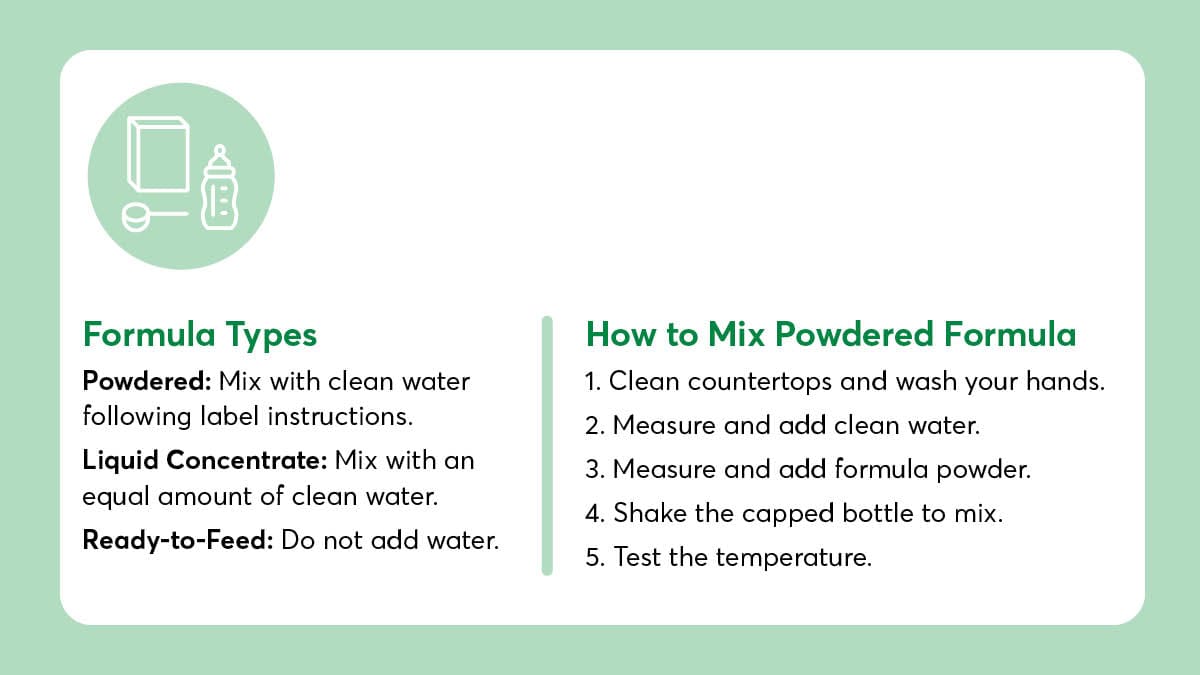
All baby formula can be divided into three categories:
• Liquid: A concentrated liquid formula that needs to be mixed with an equal amount of water before offering to your baby. Once opened, it should be stored in the fridge and used within 48 hours.
• Powdered: Needs to be mixed with a specified amount of water (following label instructions) in a bottle before offering to your baby. Once the can is opened, it should be used within one month.
• Ready-to-feed: Comes in pre-portioned 2-ounce or 8-ounce bottles or 32-ounce bulk sizes, and is ready to be fed to your baby: do not add water. Once opened, it should be stored in the fridge and used within 48 hours.
Powdered formula, while convenient and shelf-stable, is not considered sterile. Though rare, powdered infant formula can come with a risk of infection from the bacteria Cronobacter sakazakii, which can thrive in dry places, like formula powder. You might remember that Cronobacter infection was one of the primary factors in the 2022 infant formula shortage. Now, the Centers for Disease Control and Prevention recommends using ready-to-feed infant formula for babies under 2 months old, for those born prematurely, or for those with weakened immune systems.
It’s also worth noting that ready-to-feed and liquid formula varieties tend to be much more expensive than powdered options. They need to be used quickly, which may not be ideal for some families.
Beyond format, there are a variety of types of baby formula you might see on the shelves: Some formulas use different protein bases, while others are designed for particular digestive needs. Below are a few of the most common types of formulas:
Cow's Milk-Based Infant Formula
Traditionally, infant formula uses a cow’s milk base, as cow’s milk is high in lactose and shares other similarities with breast milk. However, cow’s milk differs from breast milk in protein ratios and type. Whereas mature breast milk contains a 60-to-40 ratio of whey protein to casein protein, cow’s milk contains a 20-to-80 ratio of whey protein to casein. Some formula companies add more whey protein to their cow’s milk formulas to better match the ratio seen in breast milk, in an effort to improve digestion.
Goat Milk-Based Infant Formula
Goat milk-based infant formulas are relative newcomers to the U.S. market, but have long been popular in other parts of the world. The AAP now recognizes goat milk-based infant formula as a first-line alternative to breast milk for infant feeding, alongside cow’s milk- and soy milk-based infant formulas. Because goat milk features a different type of protein structure that’s more similar to breast milk than cow’s milk is, it’s thought that goat milk formula may be easier to digest than cow’s milk formula for some babies. Still, we currently only have in vitro clinical studies to rely on for evidence at this time.
Goat milk formula may not be a solution for infants diagnosed with CMPA, given the similarities between cow’s milk and goat milk proteins. Talk to your child’s pediatrician about formula options that are safe for babies with CMPA.

Soy-Based Infant Formula
Infant formulas made from soy are the only plant-based infant formula option approved for use in the U.S. They contain a soy protein (soy protein isolate) and usually feature a non-lactose carbohydrate source, like glucose or sucrose. Soy formulas are typically recommended for babies who have galactosemia, a hereditary condition in which they cannot digest lactose—though this is rare. Most infants are born with the ability to digest lactose, says Young.
But for those who have been diagnosed with CMPA, soy formulas may not be the best choice, as an allergy to soy protein has also been found to occur in around 50 percent of babies with CMPA. Instead, your pediatrician may recommend an extensively hydrolyzed or amino acid formula (see more below). Check in with your doctor if you’re curious about soy formula.

Partially Hydrolyzed Infant Formula
Partially hydrolyzed infant formulas feature proteins that are already broken down into smaller pieces. “They can be helpful for a variety of issues that may cause general digestive discomfort,” says Young. She adds that research shows they may be especially useful if your baby is dealing with eczema. “However, they are not universally recommended, as most babies digest standard formulas made with intact proteins just fine.”
But if your infant is showing signs of formula intolerance, like excessive crying or fussiness after feeding, increased gas, loose and watery stools, eczema, or extreme fatigue, weakness, or vomiting, it’s worth talking to your child’s doctor about trying a different formula, says Sarah Sams, MD, FAAFP, and a member of the American Academy of Family Physicians board of directors. “I tell my patients to watch for any behaviors or moods that seem out of the ordinary,” Sams says. She also says that sometimes babies have reflux that may be unrelated to an intolerance. Your doctor can offer more specific guidance on infant reflux.
Using a partially hydrolyzed formula may help relieve some of that digestive discomfort, but there is only limited scientific evidence that they work well. Some partially hydrolyzed options use the terms “gentle” or “sensitive” on the label, but these aren’t regulated terms, and Young recommends parents ignore them. “They don’t have any formal meaning,” she says. “The word ‘sensitive’ on formula can mean that the formula is lactose-reduced, or it can mean the protein comes from an A2 cow"—a cow with a genetic mutation that produces milk with a different type of dominant protein known as A2 beta casein, thought to be easier to digest— "or it can mean anything,” she says. “This can obviously cause a lot of confusion for parents.”
Instead, she suggests turning to the back of the can to check the ingredients label for the term “partially hydrolyzed” listed in front of the protein source, for example, “partially hydrolyzed whey protein.”

Extensively Hydrolyzed Infant Formula
Other formulas feature fully hydrolyzed proteins, which means the proteins are broken down into even smaller chains (peptides), making them easier for a baby to digest if they’re having more severe allergic reactions. These hydrolyzed proteins are “predigested” so they won’t trigger an allergic response in kids with CMPA, making these formulas hypoallergenic. (You may see “hypoallergenic” or “HA” on the front of the can.)

Specialized Infant Formula
For babies with specific health conditions, a specialty formula may be prescribed by your pediatrician. Some of these formulas contain only free amino acids (the most basic protein building blocks, which can’t be broken down any further), rather than peptide chains, and are designed for infants who cannot tolerate other types of formula. Specialized formulas are considered a medical food and should only be used under the direction of your pediatrician, who will recommend the specific feeding amounts, schedules, and preparation instructions necessary for your baby.
How to Read a Baby Formula Label
Looking at the ingredients list on a can of formula might feel daunting: the font is so tiny, and there are just so many complex scientific names. But this spot “is where you want to go to make your decision,” says Young, who suggests focusing only on the first few ingredients in the list. “This is where 98 to 99 percent of the formula comes from,” she says. “These ingredients will be the source of digestive comfort or discomfort.”
For example, Young says, if you’re looking for a formula with a high whey content, then look for the word “whey” higher up in the list of ingredients. Paying attention to these macronutrients can help you find the right protein, carbohydrate, and fat combo that keeps your baby comfortable.
Ingredients are listed by amount, from most to least.
Macronutrients (protein, fats, carbs) make up most of what’s in the can.
Added vitamins, minerals, and other ingredients, like probiotics and prebiotics, appear after the “less than 1% line.”
The “use by” date is usually on the top or bottom of the can.
required by FDA
in the ingredients list
required by FDA
in the ingredients list
required by FDA
in the ingredients list

Photo: Getty Images Photo: Getty Images
How to Choose a Baby Formula
When it comes to choosing the “best” baby formula, three factors are key: safety, affordability, and accessibility. After all, what good is a baby formula that stretches your budget or that never stays in stock? As for safety, you can check CR’s top choices for infant formula with low or no contaminants here.
But when you’re deciding between a few brands, or even if you’re just starting out in your search for baby formula, checking in with your pediatrician or family physician is always a good idea. “We’re here to cut through the noise and give you tangible, actionable advice that keeps you and your baby’s health history and lifestyle in mind,” says Sams. So be sure to reach out with any specific questions about your little one.
Here’s what else to know about choosing a formula:
Brand-name and store-brand formulas are more similar than different. Young says that there can be minor differences between name-brand formulas and the store-brand version of that formula, but what matters most is how well your baby tolerates it. It’s also important to point out that all store-brand formulas are made by the same formula manufacturer: Perrigo. “This means that one store brand’s ‘Gentle’ formula is exactly the same as another store brand’s ‘Gentle’ formula,” Young says. “This is great news because it allows parents to shop sales and save some money.”
“Organic” doesn’t necessarily mean better. Under USDA organic guidelines, organic formulas are subject to additional restrictions, which means they must be free from certain synthetic pesticides and fertilizers. However, this doesn’t necessarily mean they’re free from contaminants like PFAS or heavy metals, which abound in our environment, and sadly, are pervasive in our food supply. While it’s difficult to avoid toxins altogether, to limit exposure, look for a formula brand that conducts third-party testing on their products and is transparent about their manufacturing safety measures and product testing.
Think about how you’ll shop for formula. If the formula you’re considering using is only available by ordering it online or driving to the bigger store in the next town over, it may not be the most accessible option. Instead, look for options that are readily available locally (consider the inevitable late-night formula run!) or investigate whether a subscription or other delivery model would work for you. Buying large quantities of formula in bulk typically isn’t recommended, since the formula could expire before you have a chance to use it.
Consider cost. There’s no getting around it: Formula is expensive—and babies drink a lot of it. If you can save some dollars by choosing a store-brand formula (several store brands topped our list of safer formula choices), your wallet may be happier.
Take marketing claims with a grain of salt. Label claims are often unregulated and undersubstantiated. Young advises parents and caregivers to outright ignore the front of the formula can and warns against making a choice based on this information alone. Instead, flip to the back. “The list of ingredients is where you want to go to make your decision,” she says.
What to Know About Baby Formula Safety Regulations and Recalls
It’s understandable to want to be sure the formula you’re feeding your baby is safe—after all, babies are highly vulnerable to infection and disease, thanks to their still-developing immune systems, and their brains are growing at a rapid rate during the first months. It’s critical that babies get the nutrients they need—without contaminants or potential health hazards.
Rest assured that infant formula is highly regulated when it comes to safety. As a food source, it falls under the Federal Food, Drug, and Cosmetic Act. And because it’s used by infants, it is subject to additional safety requirements, like bacterial testing.
“Safety is tightly regulated by the FDA, and infant formula manufacturing plants have tight safety guidelines in place,” says Young. The FDA requires formula companies to test finished products for harmful bacteria like Cronobacter and Salmonella, and any water used in the preparation of infant formula must meet safety standards set by the Environmental Protection Agency.
However, the FDA does not have much oversight in other areas of formula production. The agency doesn’t have the authority to require formula manufacturers to test ingredients or finished products for contaminants such as heavy metals, chemicals such as PFAS and bisphenols, and other toxins.
A recent Consumer Reports investigation found “potentially concerning” levels of heavy metals like lead in some infant formula samples. However, approximately half of the tested powdered formula samples did not contain worrisome levels of lead or arsenic. This shows that producing safer infant formula is achievable and highlights the need for lawmakers and regulators to strengthen existing requirements. The FDA recently announced the launch of Operation Stork Speed in an effort to improve infant formula availability and safety, and has pledged to start a nutrient review process for infant formula in the coming months.
It’s crucial to understand that making your own baby formula is not safe. Homemade baby formula can lead to serious nutrient deficiencies or an excessive intake of specific vitamins and minerals, which can harm your baby’s health and affect their growth and development.
Here’s what else to know about infant formula safety regulations:
All formulas sold in the U.S. have been shown to help babies grow. Before a company can sell a new formula, it must demonstrate through a clinical study that it supports infants’ “normal physical growth."
Formulas must meet FDA guidelines, but recalls can happen. While formula is not technically considered “FDA-approved”, all formulas must comply with nutrient and labeling requirements. Formula makers must undergo annual FDA facility inspections to test for the presence of bacteria. If a product is considered unsafe, the manufacturer is required to initiate a recall.
“Powdered infant formula is not sterile, and we do still occasionally see formula recalls. But usually, these are rare,” says Young. Recalls can be triggered by bacterial contamination, foreign objects, or other safety concerns.
Most baby formula in the U.S. is made by four companies. Those are: Abbott Nutrition (which makes Similac), Mead Johnson (which makes Enfamil), Perrigo (which makes numerous store-brand formulas, along with Dr. Brown’s and Earth’s Best), and Nestlé (which makes mostly specialty formulas). Together, these manufacturers produce around 90 percent of infant formula in the country. Smaller manufacturers include Bobbie (which makes both Bobbie and Baby’s Only; made in the U.S.), ByHeart (made in the U.S.), Kendamil (made in the U.K.), Kabrita (made in the Netherlands), and Bubs (made in Australia).
The FDA is taking steps to keep formula safe, but experts say there’s more to do. In 2022, a Similac formula recall led to the temporary shutdown of Abbott Nutrition’s largest formula plant, and combined with pandemic-era supply chain issues, resulted in a country-wide infant formula shortage that left parents and caregivers scrambling to find enough formula to feed their babies. Consumer Reports reported that in 2023, the FDA outlined industry best practices in an open letter to formula manufacturers and, soon after, sent warning letters to three manufacturers. But the agency isn’t authorized to require adherence to those guidelines.
Toddler formula is not subject to the same safety standards as infant formula. “Be sure to purchase an ‘infant formula’ for babies under 12 months,” Young says, as toddler formulas can have different levels of nutrients or added sugars and may not be suitable to support an infant’s healthy growth in the first year of life. In most cases, experts don’t recommend toddler formula for babies over 12 months, either. For more on this, see the “What to Know About Toddler Formulas” section below.
What to Know About European Baby Formulas
If you’re interested in a European formula for your baby, know that many European baby formulas don’t meet FDA labeling or nutrient requirements, which could pose a safety or health risk. During the infant formula shortage of 2022, the federal government temporarily allowed some European formulas to be sold in the U.S. market under a special provision as a stopgap.
Several of those formulas are now legally available in the U.S. full-time, says Young, and you can now also find some U.S. formulas that follow European regulations. “These are better options compared to European brands that are not officially in the U.S. and that can only be purchased through third-party websites,” says Young. “It can be hard to know how these formulas are imported and if they have been stored appropriately to ensure safety.” Finally, if you’re using a formula that’s not regulated in the U.S., you might miss out on important recall information, she says.
Best Practices for Formula Feeding
Download CR’s guide to formula feeding.
How Much Formula Does My Baby Need Each Day?
The amount of formula your infant needs each day depends on their age, weight, and general health. The AAP recommends that parents practice responsive feeding, offering bottles on demand in response to a baby’s hunger cues, in an effort to let babies regulate their own intake. Your best resource for determining how much formula your baby needs each day and their ideal feeding schedule is your pediatrician or family physician, but as for general guidance, according to the AAP, here’s what you may be able to expect for a healthy, full-term infant:
- Week 0 to 1: About 1 to 2 ounces per feed, with feedings on demand.
- Weeks 1 to 3: Your baby may start to gradually eat more, up to 3 to 4 ounces per feed, totaling about 32 ounces per day.
- Weeks 3 to 4: By the end of the first month, they should consistently take in 3 to 4 ounces per feed, with feeding sessions every 3 to 4 hours.
- Month 6: Your baby may eat 6 to 8 ounces per feeding, with 4 or 5 feedings per 24 hours.
As a reminder, this is just general guidance. Parents and caregivers should follow an infant’s hunger and fullness cues to guide their specific feeding schedules and amounts.
What to Know About Combination Feeding
You may have heard the term “combination feeding” or “combo feeding,” which means doing a mix of breastfeeding (or feeding expressed milk) and formula feeding. Combination feeding has become more normalized recently, says Kaia Lacy, CLC, a lactation consultant and low milk supply specialist who runs the virtual practice lowsupplymom.com. But it can look different for every family.
Before getting started with a client, Lacy works to understand what goals a family has in feeding their baby. Some may want to keep their breast milk supply up as much as they can while supplementing with formula, she says. Others may hope to breastfeed for certain feeds and formula-feed for others. Or they may want formula to be the primary nutrition source, and nursing will be for comfort. The best approach to combination feeding will depend on your family’s unique situation.
Lacy finds that the decision to incorporate formula is a complex one for many of the families she works with, who may combo-feed their babies after planning to exclusively breastfeed. “There’s a pervasive notion that breastfeeding is all or nothing,” she says. “There’s still this idea that you either exclusively breastfeed or there’s no point in breastfeeding at all.” Lacy likes to remind people that “any amount of breast milk means you’re breastfeeding, and that formula is an amazing, life-saving tool that makes breastfeeding accessible for a lot of us.”
There’s also some fear that by incorporating formula into feeding, you won’t be able to breastfeed anymore, as breast milk supply naturally fluctuates with changes in demand. If you’re incorporating more formula feeding and breastfeeding less, your body may start to produce less breast milk. “It’s a valid concern, and in all honesty, if we don’t have the right information as to how to complement individual lactation while formula feeding, it can lead to unintended weaning,” Lacy says. That’s where working with a lactation consultant can be especially helpful, as they can offer advice on how to stimulate milk production and share pumping tips. “With the right information and knowing what practices can complement lactation, you can breastfeed long-term even if you’re also formula feeding. My last child started formula the day she was born, and I nursed her until she was 3 years old. It’s not all or nothing,” Lacy says. If you’re looking to get started with combination feeding, reach out to a combo-feeding-friendly lactation consultant for support—many are in-network with a number of insurance providers.

Photo: Getty Images Photo: Getty Images
Tips for Transitioning to Formula From Breast Milk
Whether you’re considering supplementing breastfeeding or fully transitioning to formula for your baby, here’s what to keep in mind.
There’s no one formula that’s ‘closest to breast milk.’ “I know that a lot of marketing in recent years has focused on ‘closest to breast milk,’ but formula isn’t breast milk, and that’s OK. It’s the only human milk substitute that we know helps our children grow and thrive when breast milk isn’t available for whatever reason,” says Lacy, who focuses on accessibility and each family’s preferences when choosing a formula with her clients. Just like Young, she recommends looking at the ingredients list to see the breakdown of carbs, fats, and proteins in the formula you’re considering.
Time your feeding sessions with care. “Part of the transition from exclusive breastfeeding to combo-feeding entails some weaning, but the trick is not to wean beyond what you’re hoping to,” says Lacy, who recommends taking it slow and watching for the effects on your milk supply—especially if you’re moving ahead without designated lactation support. You can start by introducing a formula bottle in the late afternoon or early evening, when prolactin levels (the hormone primarily responsible for milk production) are naturally lower. “You’ll generally observe what impact the bottle has on supply within three to five days,” Lacy says, at which point you could start to swap out another breastfeeding or pumping session for formula.
Offer similar amounts of breast milk and formula. “Bottle volumes should be in line with what a breast milk feed volume would be, which varies by age,” says Lacy. But feeding timing may be slightly different. Because breast milk tends to be digested faster than formula, breastfed babies take more frequent feedings, such as every 2 to 3 hours, whereas formula-fed babies may stretch out feedings to every 3 to 4 hours. Talk to your lactation consultant or doctor to find a schedule that works for you.
When it comes to weaning, take it slow (if you can). When weaning fully from breast milk to formula, allow yourself plenty of time for the transition—at least a week, Lacy says, if not longer. “Sometimes, weaning can bring up difficult emotions, and there’s a hormonal shift that occurs during weaning, so I like to encourage a more extended goal timeline of two to three weeks if it’s something a person is open to in order to make that transition a little less jolting,” says Lacy. That gradual slowdown is also crucial for helping to prevent mastitis, an inflammation in breast tissue that can sometimes turn into an infection, which can be serious. A lactation consultant can help with weaning, too.
How to Switch Formulas
Switching formulas can feel fraught—babies’ delicate digestive systems can be sensitive to shifts. But sometimes you have no real choice in the matter: Maybe your baby isn’t tolerating their current formula well, or maybe the formula isn’t as accessible or affordable as you had hoped. Whatever the reason, sometimes a switch can’t be avoided.
“Switching formulas can be stressful,” says Sams, “but it’s a good idea to consider trying a new formula if your baby is always fussy, needs more iron, or has certain food allergies.” She recommends talking to your child’s doctor before making a switch. “They can help you come up with a plan to switch formulas together.”
As far as actually offering a new formula to your baby? Most babies do fine switching between formula brands when needed, according to the CDC. It’s not necessary to transition gradually, especially if your little one may be allergic to their current formula.
What to Know About Toddler Formulas
Many infant formula companies also produce toddler formulas, which are designed for children over 12 months of age. But the AAP doesn’t recommend them in most cases, saying that they’re “generally unnecessary and nutritionally incomplete,” with “questionable marketing practices.” For formula-fed babies over 12 months, the AAP instead recommends transitioning to whole cow’s milk as a beverage alongside solid food. If that’s not an option for your child, talk to your pediatrician about a plant-based choice, such as soy protein.

Photo: Getty Images Photo: Getty Images
FAQs About Formula Feeding
What Water Should I Use for Formula?
When making a bottle of formula for your baby, you’ll want to use clean drinking water. If your tap water is safe to drink, you can use that to prepare your baby’s bottle, following the manufacturer’s instructions. If you’re using powdered infant formula for babies under 2 months old or for those who may be more susceptible to illness, it’s important to take extra precautions. In these cases, boil the water first, then let it sit for 5 minutes before mixing in the formula. After mixing, allow the formula to cool to a safe temperature before feeding your baby. Alternatively, using a ready-to-feed formula is a good option.
When Do Babies Stop Drinking Formula?
The AAP recommends that babies who are drinking infant formula can transition to whole cow’s milk after the age of 12 months, as they should be able to meet their nutritional needs through solid foods and cow’s milk alone. Toddler formulas generally aren’t necessary for most children, and AAP tends to warn against them, but speak to your child’s doctor if you have questions.
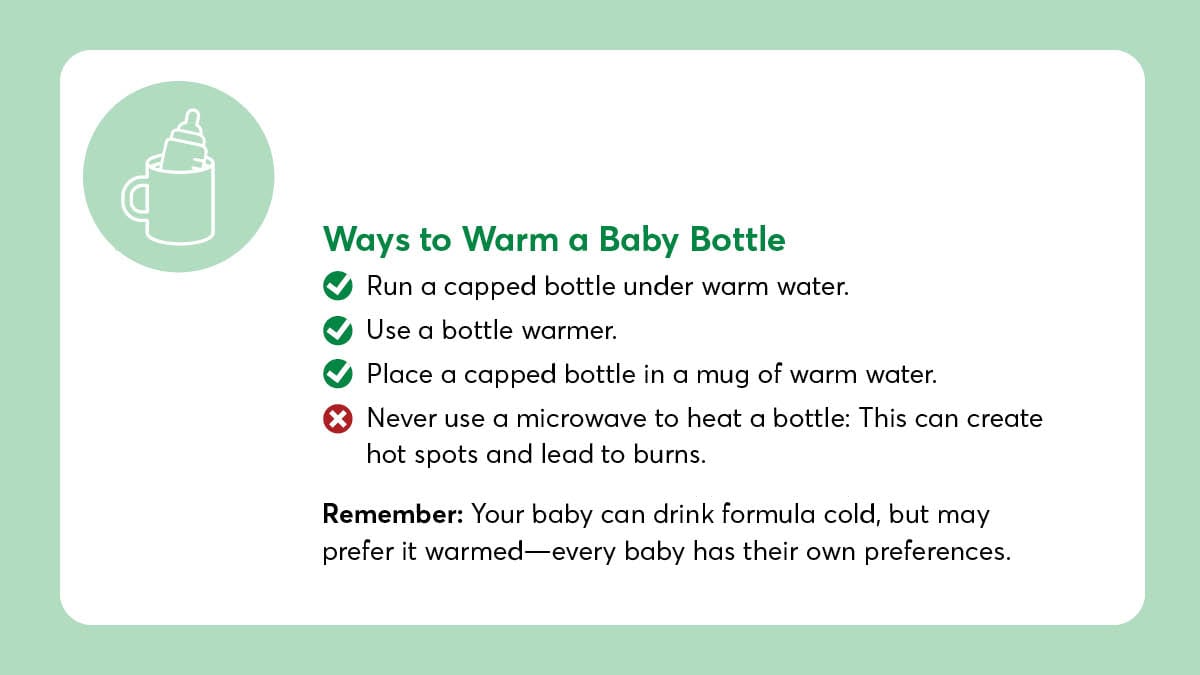
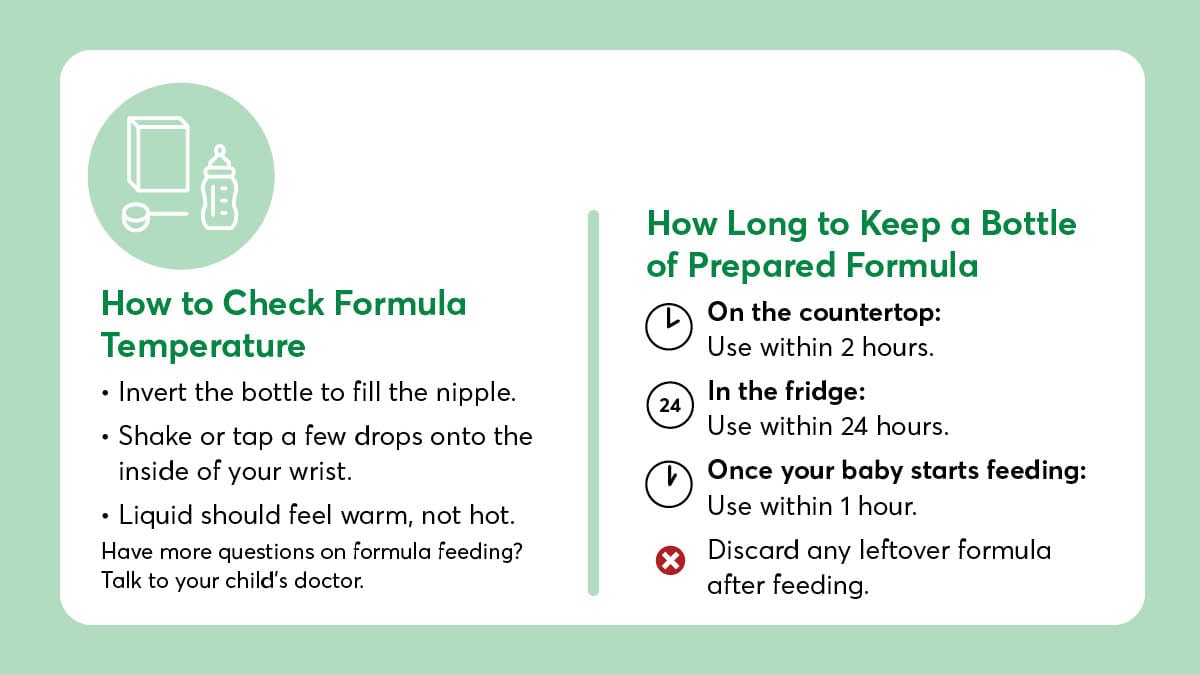
Can Babies Drink Cold Formula?
Yes. Babies can drink cold formula, but your little one may prefer it warm, especially before sleeping. To warm a bottle, hold a capped bottle under warm running water, testing the temperature before feeding by placing a couple of drops on the inside of your wrist to see if it’s too hot. Alternatively, you can use a bottle warmer. Remember never to use a microwave to heat a baby’s bottle, which can create hot spots and lead to burns.
How to Store a Bottle of Formula
The general rule of thumb for storing a bottle of prepared powdered or liquid concentrate formula is as follows:
- On the countertop: Use within 2 hours
- In the fridge: Use within 24 hours
The timing is slightly different for ready-to-feed formula. Once opened, follow the guidelines below:
- On the countertop: Use within 2 hours
- In the fridge: Use within 48 hours
You should always use prepared formula within one hour of starting the feeding. Discard any leftover formula after feeding. To store a bottle of breast milk, different rules apply.
Baby Formula Brands
A2 Platinum baby formula features a specific type of cow’s milk protein known as A2 beta-casein, which may support easier digestion.
Baby’s Only offers organic, non-GMO formulas free from corn syrup and palm oil. It’s owned by Bobbie and made in the USA.
Bobbie infant formula is produced in the USA and modeled after European infant formulas. It’s USDA-certified organic and formulated without corn syrup, soybean oil, or palm oil.
Made in Australia, Bubs provides a range of cow’s milk and goat milk formulas.
ByHeart formula is made with whole cow’s milk and is produced in the USA in a company-owned facility.
Dr. Brown’s Good Start baby formulas are produced by Perrigo and are designed to be gentle on sensitive tummies.
Earth’s Best offers organic and non-GMO baby formulas with no added corn syrup.
Elecare is an amino acid-based specialty infant formula designed for babies with severe food allergies.
Enfamil formulas are produced by Mead Johnson.
The German brand HiPP is known for its biodynamic infant formulas that promote sustainable farming.
All formulas produced by the Swiss brand Holle carry the Demeter certification for biodynamic farming, which is a highly regarded designation for sustainable farming.
Kabrita’s goat milk-based formulas are produced in the Netherlands.
Made in the UK, Kendamil uses whole cow’s milk as its base and does not contain palm oil or soybean oil.
The formula from Costco store brand Kirkland Signature is produced by Perrigo.
The store brand of Sam’s Club, Member’s Mark formula is produced by Perrigo.
Neocate is a hypoallergenic, amino acid-based specialty formula for infants with severe allergies.
Parent’s Choice is sold exclusively at Walmart and is produced by Perrigo.
Similac baby formula is produced by Abbott Nutrition.
Up & Up formula is sold exclusively at Target and is produced by Perrigo.