Colonoscopy Prep Just Got Easier
The updated guidelines should make getting a colonoscopy a bit more comfortable

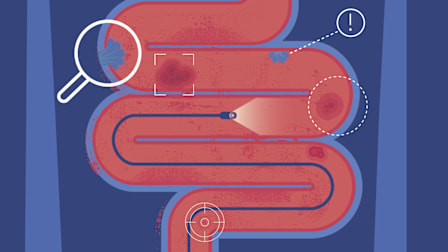
Colonoscopy prep, which involves drinking a liquid that helps evacuate your bowels, gives your doctor the best possible view of your colon during colorectal cancer screenings. But the process has long had a bad reputation—for good reason: People have had to abstain from consuming anything except liquids for a full day, and then swallow about a gallon of an unpleasant-tasting drink.
In April 2025, the U.S. Multi-Society Task Force on Colorectal Cancer released updated guidance that offers a potential reprieve, with new recommendations that should make prep easier and a bit more comfortable. Here’s what to know.
Less Liquid and More Food
The biggest change is a stronger recommendation for a lower volume of prep fluid. It turns out that for most people, less fluid—typically 2 liters—is enough to be effective, says Brian Jacobson, MD, the director of program development for gastroenterology at Massachusetts General Hospital in Boston and a co-author of the guidelines.
More Tips for Trouble-Free Prep
Drinking the prep liquid with a straw or chilling it in the fridge can make the taste more tolerable. Don’t add ice, Jacobson says, because drinking a lot of ice-cold liquid could lower your body temperature. Sip in small amounts to prevent nausea. Rather than chugging from the jug, try downing a cup every 10 or 15 minutes, says Audrey H. Calderwood, MD, a gastroenterologist and director of the Comprehensive Gastroenterology Center at Dartmouth-Hitchcock Medical Center in N.H.
As for the inevitable bathroom trips: Wear loose-fitting pants. And Jacobson suggests applying a bit of petroleum jelly to the anal area with toilet paper to reduce irritation.
Should You Try a Stool Test Instead?
If you prefer not to have a traditional colonoscopy, you can take a stool test, which screens for colon cancer by looking for hidden blood or DNA abnormalities in a sample you collect at home and send to a lab for analysis. These include the fecal immunochemical test (FIT) and the multitargeted stool DNA or RNA tests (such as Cologuard and ColoSense) with FIT.
But you’ll need to test more frequently, every one to three years instead of every 10 years for a colonoscopy. Anyone with an abnormal stool result will need to get a colonoscopy anyway. And false positives on stool tests are more common among older adults, says Calderwood.
But any screening is better than none. "Your primary care doctor can help you determine the best test for you," she says.
Editor’s Note: This article also appeared in the January 2026 issue of Consumer Reports On Health.