Sign In


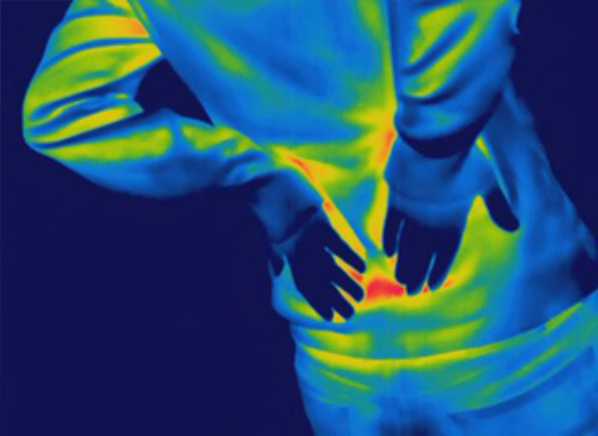
Opioid pain medications such as Oxycontin, Percocet or Vicodin work well to alleviate severe, short-term pain—due to surgery or an injury, for example—as well as pain from a terminal or serious illness, such as cancer. Doctors also commonly prescribe opioids to treat longer-term pain such as arthritis, lower-back pain, neck, or nerve pain.
But there's a surprising lack of medical evidence that opioids help much with pain lasting three months or longer, and strong evidence that long-term use carries serious risks, according to a recent, comprehensive report from the National Academy of Sciences. For that reason, recent guidelines from the Centers for Disease Control and Prevention (CDC) as well as other major medical organizations recommend against relying on opioids for routine treatment of chronic pain.
The Dangers of Pain Pills - Why you should be cautious with these powerful drugs
Besides not working well long-term to relieve chronic pain, opioids commonly cause side effects, including constipation, nausea, and drowsiness or a "fuzzyheaded" feeling. In addition, using the drugs longer term or taking higher doses can also lead to addiction, overdose, and even death. Because of these factors, Consumer Reports Best Buy Drugs has not chosen any opioid as a "Best Buy."
Instead of opioid pain medication, our medical advisers recommend first trying other treatments for chronic pain. For certain conditions such as fibromyalgia, migraines, or nerve pain, other prescription medications typically work better than opioids to control pain, and are safer.
And for other types of long-term pain, such as joint pain, over-the-counter pain relievers such as acetaminophen (Tylenol and generic), ibuprofen (Advil and generic), or naproxen (Aleve and generic) can often provide sufficient relief. Most importantly, there's mounting scientific evidence that nondrug approaches can relieve pain as well or better than medications with far less risk. For example, based on a review of the evidence, the American College of Physicians recently issued new guidelines for back pain treatment, noting that the first line of defense should be nondrug measures.
That advice is supported by a recent nationally representative Consumer Reports survey of 3,562 back-pain sufferers. It found that a higher percentage of people who participated in yoga or tai chi, had spinal manipulation, or saw a massage therapist or physical therapist, said the advice or treatment was helpful, compared with those who said they saw a doctor.
Our report details pain-relief approaches, such as acupuncture, biofeedback, chiropractic care, cognitive behavioral therapy, exercise, and physical therapy that mightc provide as much or more long-term relief than an opioid, with far less risk.
Some opioids, such as codeine and morphine, are derived from poppy plants. Others are synthetic or partly synthetic, meaning they are chemically manufactured. Some are available in combination with other pain relievers, usually acetaminophen or aspirin. Others are available as single-ingredient products.
All opioids attach to certain receptors in the brain and spinal cord, and inhibit or change pain signals. Opioids also affect parts of the brain that control breathing and blood pressure. The drugs cause people to feel sleepy or sedated, and to breathe more slowly. Over time, slowed breathing could damage the heart and lungs because those vital organs don't get enough oxygen.
Opioids can also trigger or worsen sleep apnea, a condition in which people stop breathing for short periods during their sleep.
Most seriously, opioids can cause breathing to stop completely, leading to death. That risk is greatest when the drugs are taken at high doses or combined with alcohol, sleeping pills, or other medications that make you feel sleepy.
Because opioids can be addictive and carry a potential for abuse, the federal government classifies the drugs as controlled substances and regulates prescribing. This means healthcare providers as well as pharmacies and government agencies monitor opioid prescriptions quite closely.
Below is a list of the most commonly prescribed opioids, in both short- and long-acting forms, and versions available as singleingredient drugs and in combination with acetaminophen or ibuprofen.
What you need to know about opioids - 5 surprising facts
Here's the list of some the most commonly prescribed opioids, in both short- and long-acting forms, and versions available as single ingredient drugs and in combination with acetaminophen or ibuprofen:
Generic Name(s) |
Brand Name(s) |
Available as a Generic? |
Buprenorphine |
Belbuca (patch ) |
No |
Codeine |
Generic only |
Yes |
Fentanyl |
Actiq (lozenge), Duragesic (patch), |
Yes |
Hydrocodone |
Hysingla ER, Lortab*, Norco*, Yes |
Yes |
Hydromorphone |
Dilaudid, Exalgo |
Yes |
Levorphanol |
Generic only |
Yes |
Meperidine |
Demerol |
Yes |
Methadone |
Dolophine, Methadose |
Yes |
Morphine |
Avinza ER, Kadian ER, MS Contin CR, Oramorph SR |
Yes |
Morphine plus naltrexone |
Embeda ER |
No |
Oxycodone |
Oxycontin ER, Percocet*, Roxicodone, Roxicet*, Endocet*, Xtampza ER |
Yes |
Oxymorphone |
Opana, Opana ER |
Yes |
Tramadol |
ConZip ER, Ultram, Ultracet* |
Yes |
CR=controlled release; SR=sustained release; ER=extended release
* These versions contain acetaminophen.
** These versions contain ibuprofen.
Starting in the 1990s, many physician specialty groups and government agencies supported expanded use of opioids to treat long-term pain. Yet, as opioid sales have quadrupled since 1999, there's been no overall reduction of pain in the U.S., according to the CDC.
In fact, research shows that Americans report more long-term pain than people in other countries where people use far fewer prescription opioids.
At the same time, skyrocketing use of opioids has led to an alarming rise in fatal overdoses, which reached a record of more than 33,000 in 2015, according to the most recent data from the CDC. Nearly half of those overdose deaths involved prescription opioids. The CDC has alerted consumers and healthcare professionals about these key issues:
Studies have not proven that opioids work well to alleviate pain, help people move easier, or improve quality of life when used long term.
That's the case, even for people who use them to treat pain. Studies show that up to one out of four people who take opioids for pain wind up misusing the drugs—taking larger doses or taking them more frequently than prescribed, for example—or find that the drugs interfere with their daily life, according to the recent National Academy of Sciences report. You're at greater risk for addiction if you've had anxiety, depression, or other mental health disorders or if you or a close family member has a history of substance abuse.
Most people develop a tolerance to opioids, meaning that it takes larger and larger doses over time to get the same effects. And taking such doses increases the risk of dangerous side effects, including accidental overdose.
Nearly everyone who takes opioids for longer than a couple of weeks becomes physically dependent on them. That can make it hard to stop taking the drugs without suffering unpleasant withdrawal symptoms, including insomnia, anxiety, and muscle aches.
Mounting evidence of the limited benefits and potential harms of opioids when taken longer term has led to a change in thinking about how to use these powerful drugs. Today, the CDC and other organizations are recommending that healthcare providers prescribe opioids for chronic pain only as a last resort, after trying other medications and nondrug approaches.
Read the latest advice from the CDC about treating chronic pain with opioids.

If you are diagnosed with chronic pain, the first decision is whether to take pain medicine at all. Since pain is a highly personal experience, only you and your doctor can reach this decision. Pain specialists now emphasize that some people with chronic pain can manage well without taking any pain medicines regularly. And, others may experience improvements in pain and ability to function with nondrug treatments, including exercise, lifestyle adjustments, behavioral therapy, acupuncture, and massage.
If you have bothersome pain despite nondrug measures, you and your doctor may consider treating it with a medication. Talk to your healthcare provider about the risks and benefits of different types of pain drugs in light of your individual symptoms and medical history. Ask how much relief you might expect over the long term, what side effects to be alert for, and what steps to take if the drug doesn't help.
Based on current research, an opioid is usually not the best, first choice for pain relief. Instead, for most types of longterm pain, Consumer Reports Best Buy Drugs recommends trying acetaminophen first. One exception is chronic back pain, which research now shows may be better relieved by an anti-inflammatory drug (see below).
When taken as directed, acetaminophen has a long track record for safety and, even at moderate doses, can be quite effective. In addition, it's available without a prescription and is inexpensive.
Use the lowest doses of acetaminophen that provide adequate pain relief—Consumer Reports medical advisers suggest no more than 3,250 mg of the drug in a 24-hour period. If you find that you need to use the FDA's maximum dose (4,000 mg) for acetaminophen, or that you take it every day, consult with your doctor about the drug's link to liver damage and other problems. The risk is greater at higher doses and also in people who drink alcohol heavily, or have existing liver damage or liver disease.
Keep track of how much acetaminophen (or any pain reliever) you take. Hundreds of over-the-counter medicines contain acetaminophen, including allergy, cough and cold drugs, fever reducers, and sleep aids. Although the FDA has lowered the maximum per-pill dose of acetaminophen for prescription medicines to 325 mg, unfortunately, it hasn't taken the same step for the over-the-counter products. Extra-strength Tylenol, for example, contains 500 mg of acetaminophen.
How much acetaminophen is too much?
If your pain is not sufficiently controlled by acetaminophen, or if you have chronic back pain, consider a nonsteroidal, anti-inflammatory drug (NSAID) such as naproxen (Aleve and generic) or ibuprofen (Advil, Motrin, and generic).
Our analysis of the evidence shows that all NSAIDs are generally equally effective, although some people may respond better to one type than another. If one NSAID does not work well for you, try switching to another. And, if over-the-counter NSAIDs don't work, consider prescription celecoxib (Celebrex and generic) or meloxicam (Mobic and generic).
Aspirin is not a good choice for treating chronic pain because the larger doses typically needed to provide relief, can cause bleeding in the stomach or intestines, which can be serious. (Other NSAIDs also pose this risk, too.)
People at high risk of such internal bleeding, and those taking certain other medications, such as blood thinners, should not take any NSAID. If you take NSAIDs frequently and have stomach upset or blood in your stool, see a doctor.
NSAIDs have also been linked to a higher risk of heart disease, heart attack, and stroke, though this risk is very small. Occasional, short-term use of low doses probably does not increase that risk for otherwise healthy people. But for those who already have heart disease or who have high blood pressure, diabetes, or high cholesterol, the risk is greater.
Before you start taking an NSAID on a regular basis for chronic pain, and particularly if you take high doses, your doctor should evaluate your risk for heart disease and stroke. This is especially true for people aged 65 and older as the risk for both rises with age.
This table provides a basic overview of both acute and chronic pain treatment.
Type of pain |
Best initial treatment |
If that doesn't work + comments |
Tension Headache
|
Acetaminophen or an NSAID1
|
See a doctor if headaches are severe, persistent, or accompanied by fever or vomiting, or you have difficulty with speech or balance. Don't self-medicate for more than two weeks. Opioids rarely prescribed. |
Migraines
|
Acetaminophen, NSAIDs
|
A triptan or other preventive medication may be needed, especially if migraines are frequent and/or severe. Opioids rarely prescribed. |
Menstrual cramps |
NSAIDs |
You don't necessarily have to use a product marketed specifically for cramps; any OTC NSAID product may be helpful. |
Pain due to minor trauma (bruises, scrapes, minor sprains) |
Acetaminophen, NSAIDs
|
Opioids not recommended.
|
Pain due to moderate or severe trauma (wounds, burns, fractures, severe sprains) |
Opioids. Other drugs may be prescribed as well
|
Most people can transition to safer OTC painkillers within three days; few people will need opioids for more than a week.
|
Post-surgical pain — minor |
Acetaminophen, NSAIDs |
Opioids rarely needed. |
Post-surgical pain — moderate to severe
|
Opioids. Other drugs may be prescribed as well
|
Opioids likely to be prescribed. Most people can transition to OTC painkillers within a week.
|
Muscle aches and strains |
Acetaminophen, NSAIDs, muscle relaxants |
See a doctor if pain persists. |
Osteoarthritis |
Acetaminophen, oral and topical NSAIDs, topical preparations that provide heating or cooling sensations. |
See a doctor if pain persists. Opioids used occasionally for moderate-to-severe pain flare ups, or for chronic pain. |
Pain following dental procedures |
Acetaminophen, NSAIDs
|
Short-term use of an opioid may be needed if pain is severe.
|
Discomfort and pain due to heartburn or GERD2 |
Antacids, H2 Blockers (e.g. Tagamet, Zantac), Proton Pump Inhibitors (e.g. Prilosec OTC) |
Heartburn that lasts more than a week needs medical attention. Aspirin and NSAIDs should be avoided. |
Chronic back pain
|
Acetaminophen, NSAIDs
|
Consider the prescription pain reliever tramadol or the antidepressant duloxetine, which is FDA approved to treat chronic lower back pain. If prescribed, opioids should be part of a comprehensive treatment program that includes nondrug measures such as exercise. |
Pain from a kidney stone |
Acetaminophen, NSAIDs, Opioids |
Opioids may be prescribed if pain is severe. Studies show NSAIDs to be as effective as opioids. |
Nerve pain3
|
Acetaminophen, NSAIDs, Anticonvulsants
|
Opioids are sometimes used, but only if anticonvulsants or other drugs have been tried and don't work. Antidepressants, lidocaine patches, and capsaicin cream are other options. |
Pain due to fibromyalgia4 |
Antidepressants, Anticonvulsants |
Opioids have not proven to be effective in treating fibromyalgia. |
* Important Note: The information in this table is not comprehensive. It is meant as general guidance and reflects typical medical practice. It should not substitute for a doctor's advice. If you have pain that lasts for more than 10 days, see a doctor. The table is based on numerous sources and does not reflect analysis or input from the Drug Effectiveness Review Project. Always follow the labeling or package insert information on nonprescription and prescription drugs you use to treat pain.
1. Includes aspirin and aspirin-like drugs such as ibuprofen (Advil, Motrin, and generic) and naproxen (Aleve and generic).
2. GERD=Gastroesophageal Reflux Disease, also referred to as stomach acid reflux.
3. Associated with diabetic neuropathy, shingles, injury-related nerve damage, compression of nerves in the spine, and nerve damage associated with cancer or HIV infection.
4. Fibromyalgia is a condition marked by muscle and joint tenderness and pain. Fatigue can also be present. The cause is unknown. The symptoms it produces and their severity vary widely from person to person.

There is very little research comparing how well different types of opioids work to treat chronic pain. So, we do not know if one opioid may be better than another— either overall, or in treating certain types of pain, or treating certain people.
That said, studies do clearly suggest that when a person is given similar doses of any of the opioids, the relief a person experiences from pain is about the same. Opioids also appear to produce similar results when a person's "quality of life" is measured.
In addition, few studies have compared opioids with non-opioid drugs and none have compared the two over a long period of time.
Here are some additional important points about opioid effectiveness, use, and safety from the research literature:
Opioids don't relieve 100 percent of pain. For example, a person who has a pain score of 7 on a zero-to-10 scale could have a score of only 4 or 5 after taking an opioid. And, the amount of pain relief you experience may lessen over time. Most people who take the drugs every day develop a tolerance to them—meaning that they need a higher dose to get the same level of relief. Because the risks increase with higher doses, most doctors are uncomfortable increasing doses past a certain point.
Risk of side effects may not outweigh benefits. To get adequate pain relief, some people may have to take doses so large that risk of side effects outweighs any benefit. Even at lower doses, some people are so bothered by side effects such as constipation, nausea, dizziness, and sleepiness, that they stop taking the drug. Little is known about the long-term effects of taking opioids. Most studies evaluating opioids have lasted only three months or less—so little is known about how well they work over a longer time.
But so far, evidence on long-term use of opioids is not encouraging. For example, a recent review in the Journal of the American Medical Association of 20 trials involving nearly 7,300 patients with chronic back pain found that opioids didn't provide significant relief. Further, half the participants dropped out early because the medication didn't work or the side effects were intolerable.
Opioids can increase your sensitivity to pain. Longterm opioid use actually makes some people more sensitive to pain. The effect can be worse with higher doses—another reason why your doctor may want to limit your opioid dose.
If you don't respond to one type of opioid, or if you develop a tolerance to it, your doctor may try switching you to a different opioid. Some people simply respond better to one opioid than another, and trial and error is the only way to find that out.

Long-acting (extended-release) forms of opioid medications stay in the body longer and have more medication than short-acting versions. Many doctors prescribe long-acting opioids for patients with chronic pain because the drugs allow patients to take fewer pills for round the-clock coverage. But long-acting opioids are more likely to cause potentially fatal overdoses in some patients.
Studies suggest that short-acting opioids work just as well as long-acting, even for chronic pain. Because of that risk, the FDA has advised that long-acting drugs be reserved for only patients needing consistent, round-the-clock help, such as people battling pain from cancer or a terminal illness.

One reason for a cautious approach toward opioids is that they can cause harm. In fact, most people who take an opioid will experience at least one side effect. The most common ones include dry mouth and constipation—which can be severe and require other drugs to relieve—nausea, dizziness, lack of energy, urine retention, slowed breathing, or excessive drowsiness.
In studies, about one in five people stopped taking an opioid because of side effects. Drinking alcohol or taking certain other medications such as tranquilizers, sedatives, or antihistamines worsens some of the side effects of opioids, especially the feelings of being sedated or "fuzzy headed," as well slowing breathing. Many accidental overdoses involve the use of opioids in combination with alcohol or other drugs.
Among the most dangerous types of drugs to combine with an opioid are benzodiazepines, which are used as anticonvulsants, anti-anxiety medications, muscle relaxants, and sedatives—for example, alprazolam (Xanax and generic), clonazepam (Klonopin and generic), diazepam (Valium and generic), and lorazepam (Ativan and generic).
Some side effects, such as nausea, will ease over time, while constipation can be reduced with laxatives and stool softeners. Others, such as drowsiness and sedation may persist, and can make it difficult to do daily activities like driving or simply concentrating on a task. This can be especially true if you take higher doses.
That's why many chronic pain patients complain that even if opioids help take the edge off their pain, the drugs don't always improve quality of life. Indeed, it's why opioids can become "part of the problem" for many people with chronic pain, who previously led, or want to lead, active lives.
The box below lists common opioid side effects and adverse events.
Opioid Side EffectsSome effects may ease up over time, while others can be managed. |
|
|
|

One of the most serious concerns about taking opioids is the risk of addiction, which has increased substantially in the last decade as more people take opioids for pain treatment and as recreational use of the drugs has increased. The risks of becoming hooked on opioids, even if you use them to treat pain, is much higher than previously thought.
A recent survey conducted by researchers at the National Institutes of Health (NIH) found that more than one out of three U.S. adults took a prescription opioid in 2015. More than 12 percent of people who took an opioid—an estimated 11.5 million Americans—didn't use these highly addictive drugs as their doctors directed. That includes, for example, taking larger or more frequent doses than their doctors advised or even using opioids prescribed for someone else. Another 2 million adults had become addicted to opioids.
Surprisingly, attempting to treat pain—not a desire to achieve a euphoric "high"—was the number one reason cited for taking opioids by people who misused the drugs or had become addicted to them according to the survey.
Doctors once thought that the risk of addiction was very low for people who take opioids to treat pain. But recent research indicates that when opioids are used continuously for more than a few weeks—even when they are used appropriately to treat severe pain—people become physically dependent on the drugs and may have trouble stopping them. In addition, a higher percentage of people wind up becoming addicted to opioids than previously thought.
A recent study from the CDC found that every day you continue to take an opioid after the first few days decreases the odds that you will be able to stop taking the drugs.
Another study found that even some people prescribed opioids for short-term pain wind up getting hooked on the drugs. Researchers from the University of Michigan Medical School examined the records of more than 36,000 adults younger than 65 who underwent surgery and who had not taken opioid pain medication the year prior to their procedure. Three months after surgery, when nearly all patients should have recovered, the researchers discovered that about 6 percent were still taking opioids.
Experts distinguish between addiction, physical dependence, and tolerance.

The NIH survey reinforced findings from other research showing that people are more likely to become addicted to opioids if they have a history of depression or suicidal thoughts or if they have had a substance use disorder involving other legal or illegal drugs. But the survey results also underscored that even people without risk factors can become dependent or addicted to the drugs.
All these problems make it essential to take opioids with great care and under the watchful eye of a doctor who knows how to tell when you may be getting addicted. The signs of addiction include:
• Taking higher doses of the drug for a longer time than was originally intended.
• Craving opioids—that is, experiencing a strong desire or urge to use them.
• Spending a lot of time focused on obtaining, using, and recovering from the effects of opioids.
• Being unable to cut back or control opioid use even though the drugs are not working well for pain relief and are causing physical or psychological problems.
• Neglecting responsibilities at work, home, or school and missing out on important social and recreational events because of opioid use.
People who become addicted to opioids should seek treatment for a doctor who specializes in treating substance use disorders. We don't evaluate or compare treatments for opioid addiction here, but they include counseling and support groups as well as medications such as buprenorphine, methadone, and naltrexone that can help reduce cravings.
If your chronic pain is severe, and not well controlled with other drugs or nondrug treatments, opioids are an option to consider. But before prescribing an opioid drug, your healthcare provider will likely require some information and simple tests.
For example, you may be asked to keep a pain diary for a few weeks, rating how severe your pain is and how often you experience it. Keeping track will give your doctor more detailed information on your pain "patterns." He or she may also give you one or more tests to clarify how pain is affecting your quality of life. Your doctor is also likely to ask you about past and present drug or alcohol use, whether you have a family history of such problems, whether you are depressed or have anxiety, and screen your urine for opioids or other drugs.
Your doctor is trying to determine whether the benefits of an opioid outweigh the risks. In fact, it's your doctor's responsibility to determine if you are at high risk of becoming addicted to opioids before prescribing them.
If you wind up taking opioids for long-term pain, the CDC advises starting on the lowest effective dose of a short-acting medication, increasing the dose cautiously, if necessary, and not exceeding a pre-set limit.
Be realistic about your expectations for treatment. In the long run, the drugs will only reduce your pain by about 20 to 30 percent—or they may not help at all. Work with your doctor to set treatment goals and make a plan for what to do if they aren't met. Your healthcare provider should evaluate your progress using standard assessments of pain and function within one month of when you start taking an opioid, whenever you increase the dose, and at least every three months as long as you take the medication. He or she will also likely test your urine at least once yearly to make sure that you are taking
the medication as prescribed.
Your doctor may also ask you to sign an agreement about how your treatment with opioids will be managed. That form will likely spell out how your healthcare provider will prescribe the drugs, how you will be monitored to make sure the drugs are helping and that you are using them safely, and what signs may indicate that you need to stop using opioids or reduce your dose.
Finally, anyone who regularly takes an opioid should talk to their doctor about keeping a rescue drug, naloxone, on hand. The rescue medication can reverse a potentially fatal overdose in minutes. Naloxone comes in the form of an auto-injector or nasal spray, either of which is easy for anyone to use in an emergency. Healthcare providers can prescribe naloxone, but in most cases you can get it even without a prescription. It's typically covered by health insurance.
While we typically designate "Best Buys" for a category of drugs based on effectiveness, safety, and cost, in this case we have not chosen a Best Buy opioid for the treatment of chronic pain. That's because there's no good evidence showing that opioids are effective in treating long-term chronic pain, or that any one opioid is any better than another for that purpose.
And, the risk of addiction and overdose is too high. Indeed, our medical consultants suggest people should, in consultation with their doctors, try other pain relievers and nondrug treatments first.
That said, if you and your doctor decide you need an opioid to relieve chronic pain or a pain flare-up, we recommend generic versions of hydrocodone/acetaminophen, oxycodone, or tramadol. Our recommendations aren't based on any evidence that these opioids are better than others. Instead, they are based on cost; these generic versions cost less than $100 a month, on average.

✔ Read the label and take the drug exactly as directed. Never take more than advised, don't take it with alcohol, and don't combine it with any other drug without your doctor's OK. Most opioid deaths involve alcohol or sleeping pills.
✔ Get tested for sleep apnea. If you snore loudly, get checked for the condition, because opioids can make it worse or even fatal.
✔ Be cautious if you have a respiratory problem. Opioids can interfere with breathing if you have a cold, an asthma flare-up, or bronchitis. So let your doctor know right away, and see whether you need a lower dose until you recover.
✔ Avoid opioids if at all possible if you are pregnant or could become pregnant. The drugs slightly increase the risk of birth defects in a developing fetus as well as the risk that an infant will be born early or underweight. If a woman takes opioids late in pregnancy, her baby could be born addicted to the drugs and suffer withdrawal symptoms in the first days of life. If you are pregnant and need an opioid, talk to your doctor about taking the lowest possible dose for the shortest time.
✔ Don't drive or do anything that requires you to be fully alert. That's especially important when you first start taking an opioid or whenever you change the type or dosage.
✔ Put opioids in a locked drawer or cabinet to prevent children from taking them or others from using them for recreational purposes.
✔ Expect regular monitoring. If you take opioids, your doctor should assess you at regular visits. If pain and function do not improve after starting the drugs, then they probably are not working well enough to justify the risks. Your doctor will also monitor opioid use by testing your urine, checking your pill bottles, or checking a state database of controlled substance prescriptions.
✔ Keep nalozone on hand. The CDC, FDA, as well as many medical organizations recommend that people who regularly take prescription opioids keep naloxone, an opioid antidote that can reverse a potentially fatal overdose in minutes. Make sure that friends and family members know where you keep the rescue medication and how to use it if your breathing becomes dangerously slow or stops.
✔ Discard unused pills. Many pharmacies now take back medications, including opioids, and, in many communities, fire and police departments and hospitals also accept leftover drugs . (Read more about options for disposing of unused opioids and other medications.) If you you have no other choice, the FDA says, unlike other drugs, opioids are so risky excess pills should be flushed down the toilet.
Our evaluation of opioids in the treatment of chronic pain is based on an analysis from an independent, scientific review of the evidence on the effectiveness, safety, and adverse effects of opioids. The review was conducted by a team of researchers at the Pacific Northwest Evidence-based Practice Center at the Oregon Health and Science University in Portland and at the University of Washington in Seattle. It was funded by the Agency for Healthcare Research and Quality (AHRQ), published in October 2014 and is available here.
One of the researcher who co-authored the AHRQ report was a consultant to Best Buy Drugs in updating this report. A physician and specialist in evidence-based research and analysis who is a consultant to Consumer Reports Best Buy Drugs reviewed the AHRQ report and the initial draft of this Best Buy Drugs report and made additional suggestions for revisions. We also contracted with three additional physicians who specialize in pain care to review our report, one of whom served a peer reviewer of the AHRQ report. We thank all these contributors for their valuable assistance and attention to detail.
The AHRQ review probed in detail the findings of 39 studies that evaluated opioids in the treatment of chronic pain. But the review drew on a range of other literature. A list of references appears at the end of the AHRQ paper.
The most recent update of this evaluation reflects the following research:
• A CDC report on opioid prescribing published in August 1, 2017.
• Results from the 2015 National Survey on Drug Use and Health published in the Annals of Internal Medicine July 31, 2017.
• A Consensus Study Report from the National Academy of Sciences on pain management and the opioid epidemic published July 13, 2017.
• A study on how long term opioid use starts after surgery published in JAMA Surgery on June 21, 2017.
• Clinical Practice Guidelines from the American College of Physicians on noninvasive treatments for back pain, published April 4, 2017.
• A study from the CDC on initial prescribing and the likelihood of long-term opioid use published March 17, 2017.
• A systematic review of studies examining the use of opioids for chronic back pain published in JAMA Internal Medicine in July 2016.
• CDC guidelines on prescribing opioids for chronic pain, published in March 2016.
These materials are made possible by a grant from the state Attorney General Consumer and Prescriber Education Grant Program, which is funded by the multi-state settlement of consumer-fraud claims regarding the marketing of the prescription drug Neurontin (gabapentin).
 Build & Buy Car Buying Service
Build & Buy Car Buying Service
Save thousands off MSRP with upfront dealer pricing information and a transparent car buying experience.
 Get Ratings on the go and compare
Get Ratings on the go and compare
while you shop