Sign In

Menu
Suggested Searches
Recent Searches
Suggested Searches
Product Ratings
Resources
Chat With AskCR
Resources
All Products A-ZThe payment for your account couldn't be processed or you've canceled your account with us.
Re-activateMy account
Sign In
My account
Sign In

Back in 2007, Consumer Reports put out a call for stories about the health insurance coverage problems that consumers were facing. We received thousands of accounts of families left without coverage.
The health reforms of the Affordable Care Act have helped, creating new coverage options and closing many loopholes that left people stranded.
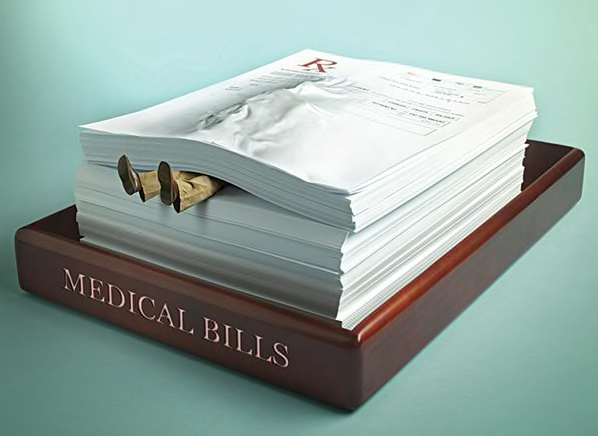
But new stories keep rolling in. We frequently hear that consumers with health insurance are getting hit by surprise medical bills after a hospital visit or planned procedure. Consumers tell us they are taking careful steps to make sure doctors and hospitals are in their insurance network—only to find out later that one of the many doctors who took part in their care was out of network.
What usually occurs in that situation is "balance billing," which allows doctors to bill patients for the portion of their charges the insurance company didn't pay under out-of-network coverage. It is legal in most states.
"Patients are confused and overwhelmed by these bills," says Blake Hutson, senior associate for health reform at Consumers Union, the advocacy division of Consumer Reports. "You're basically at the mercy of the doctor as you try to negotiate a discount on the bill or acceptance of the insurance company's coverage as payment in full."
Consumers Union is pushing for state laws that will end the practice. And we are seeing some progress. New York state's new law, which took effect April 1, bans balance billing in emergency medical situations. We think it serves as a good model for other states. Until your state acts to end surprise medical bills, take these steps to protect yourself:
—Diane Umansky
 Build & Buy Car Buying Service
Build & Buy Car Buying Service
Save thousands off MSRP with upfront dealer pricing information and a transparent car buying experience.
 Get Ratings on the go and compare
Get Ratings on the go and compare
while you shop