Sign In


For many consumers, good health care means seeing as many specialists as possible. It may also mean undergoing rounds of tests and, if a serious illness is diagnosed, prolonged hospital stays and extensive treatment.
Though the idea that more health care is better seems to make sense, recent research has shown that none of the above necessarily helps you live better or longer. In fact, too much medical care might shorten your life.
Those findings grew out of the 2008 Dartmouth Atlas of Health Care study and almost three decades of research by John E. Wennberg, M.D., and colleagues at Dartmouth Medical School. Their study of 4,732,448 Medicare patients at thousands of hospitals in the U.S. from 2001 through 2005 found significant variations in the way that people with serious illnesses such as heart failure and cancer were treated during the last two years of their lives. Some regions used two or three times the medical and financial resources than others.
Other Dartmouth research has found that patients with serious conditions who are treated in regions that provide the most aggressive medical care—more tests and procedures, more specialists, and more days in the hospital—don't live longer or enjoy a better quality of life than those who receive more conservative treatment.
Patients treated most aggressively are at increased risk of infections and medical errors that come from uncoordinated care, such as doctors prescribing drugs that duplicate or interact with other drugs. They also tend to receive poorer care, spend a lot more money for co-payments, and are the least satisfied with their health care, the Dartmouth researchers found.
The chronically ill are not the only ones vulnerable to overly aggressive care. Consider the case of a middle-aged IBM executive from the New York City area who experienced chest pain. He went to a cardiologist, who ordered a full workup, including a CT scan of his chest. The scan found no heart problem, but at the edge of the film the radiologist noticed "something funny" in the neck area. A neck surgeon performed a biopsy and found nothing wrong. The cardiologist then performed an angiogram to look for abnormalities in the blood vessels. Complications from that procedure landed the executive in the hospital for a brief period. By the time it was over, his bills were more than $150,000 and he still had no diagnosis. Eventually the pain disappeared on its own.
Months later, when the executive's chest pain returned, he told his medical history to Paul Grundy, M.D., an internist and director of health-care technology and strategic initiatives at IBM's headquarters in Armonk, N.Y. Grundy asked him what he was doing at the time. "Oh, we started gardening again," the man told him. It turned out that overzealous use of his string trimmer had strained a chest muscle, a condition that required no treatment other than an over-the-counter pain reliever. None of the high-priced specialists (some call them the "partialists") had considered muscle strain, a common condition often mistaken for heart pain.
Few Americans are aware of the dangers of this type of unneeded testing and overreliance on specialists. Instead, many fear that their health problems will be neglected or inadequately treated. But for people with good private health insurance or Medicare, the perils of overtreatment are real.
Avoiding excessive testing and hospital stays is easier in some parts of the U.S. than in others where a "do more" medical culture prevails. We worked with the researchers at the Dartmouth Atlas to make their data on 2,878 hospitals available free at ConsumerReportsHealth.org. Use the Web site to find out how hospitals in your area treat people with long-term, life-threatening illnesses. Also consult Hospital Compare to Hospital Compare, a Medicare project that rates hospitals by patient satisfaction and a variety of other measures. And no matter where you live, get the right kind of care for serious illnesses by using these tips.
The amount of medical care that people get for serious illnesses varies enormously from place to place. In the last two years of life, the average patient spent 11 days in the hospital in Bend, Ore., and 35 days in Manhattan. In those same two years, patients visited the doctor an average of 34 times in Ogden, Utah, and 109 times in Los Angeles.
The Dartmouth Atlas based those findings on the Medicare claims records of millions of patients who died from (in order of prevalence) congestive heart failure, chronic pulmonary (lung) disease, cancer, dementia, coronary artery disease, chronic kidney failure, peripheral vascular (circulatory) disease, diabetes with organ damage, and severe chronic liver disease. Together those ailments account for about 90 percent of deaths of people older than 65.
Over the years, Dartmouth research has yielded some startling insights:
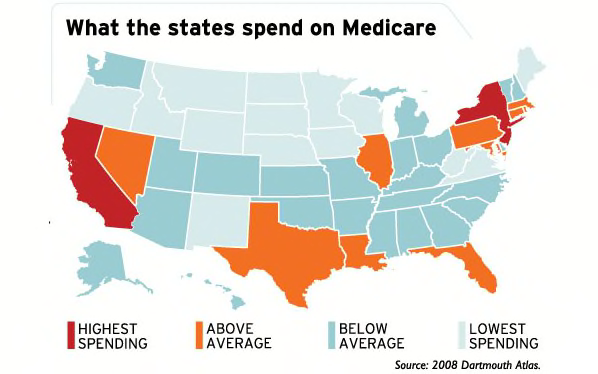
Medicare spending in the last two years of life varies almost twofold from the lowest-spending state, North Dakota, to the highest, New Jersey. Three hot spots of aggressive care: New Jersey, New York, and California.
In some areas of the country, seriously ill patients have trouble escaping futile and often painful overtreatment. Jean Callahan, a social worker and attorney with the Vera Institute of Justice, a New York City public-interest group, became the court-appointed guardian for a 90-year-old bedridden woman so completely unresponsive that Callahan never even found out whether she spoke English. She had a feeding tube, but her stomach could not process the food. Both feet and lower legs had gangrene. The woman's doctors "brought us into the case to consent to the amputation of one of her legs, but because the hospital considered the surgery to be life sustaining, we didn't really have the legal power to say no," Callahan says. "It was obvious to everyone around her that she was dying, but when we attempted to have her moved to hospice, the doctor said, 'No, I don't think she's ready.' They eventually amputated both of her legs, and she continued to get aggressive treatment, including intravenous antibiotics. In the end, she died of an infection."
So, why does the health-care system serve up so much more care in New York than in Iowa? "Doctors decide who needs health care, what kind, and how much but have surprisingly little information on what the 'right' amount actually is," says Dartmouth's Wennberg.
If a patient has heart failure, there is little valid evidence, and no clear rules, about when to ask a patient to return for a follow-up visit, when to hospitalize him, or at what point to admit him to the ICU. "When faced with the uncertainty of medicine, physicians will use available capacity up to its point of exhaustion, no matter how much capacity there is," the Atlas says.
Also, most American doctors are paid per visit, test, or procedure, rather than being on a salary. So the more they do to patients, the more money they make.
"If you live in Fort Myers, Fla., you're two or three times more likely to get your knee replaced than if you live in Miami," Wennberg says, "because there are more orthopedic surgeons in Fort Myers on the lookout for patients than there are in Miami."
The exception to this rule helps prove it. A few common conditions—fractured hips and appendicitis, for instance—have a clear-cut diagnosis, and the need for hospitalization is universally accepted. Regardless of the local supply of hospital beds, the rates of initial hospitalization for those conditions are virtually identical in all regions.
The Dartmouth Atlas ranked NYU Langone Medical Center in New York City No. 1 in the nation among hospitals/medical schools for aggressive care and spending. Its chief medical officer, Robert Press, M.D., said the hospital was concerned when rankings first came out, in the 2006 edition of the Atlas. "Following the release of the original data, we began a number of initiatives that are still ongoing toward defining the patient's wishes at the time of admission regarding the extent of care that he or she wants provided." But Press also notes that many patients and families served by his hospital "really desire very aggressive care. And a number of our physicians really believe in providing aggressive care. We are changing this to the extent it can be changed, but it is a cultural change."
Cedars-Sinai Medical Center in Los Angeles ranked second for aggressiveness of end-of-life care. Thomas M. Priselac, the hospital's president and CEO, says that while Dartmouth is doing "very important work," without more detailed hospital-specific data "it raises more questions than it provides answers."
A key question, of course, is whether patients are being kept alive longer in the regions that spend more money and deliver more aggressive care. "To judge survival, you have to look at people who are similarly ill and then follow them forward over time," says Elliott S. Fisher, M.D., Wennberg's longtime research collaborator. "And we've done that." Their study of 969,325 Medicare beneficiaries hospitalized nationwide for three common conditions—colon cancer, heart attack, and hip fracture—published in the Feb. 18, 2003, issue of the Annals of Internal Medicine, analyzed the follow-up tests and treatments the patients received for up to five years after their very similar initial treatment.
Patients in the highest-spending areas received 60 percent more treatment than those in the lowest-spending areas, but the extra care didn't seem to help at all, and it made some things worse. Patients in the high-spending, aggressive-care regions waited longer in emergency rooms and doctors' offices than patients in lower-spending regions did. They were less likely to get recommended preventive treatments, such as aspirin to prevent future heart attacks, or appropriate immunizations. They were slightly more likely to die, and those who didn't die weren't any better off in terms of their ability to function in daily life. And overall they were no more satisfied with their care.
Other research groups have had similar findings using different methods.
A state-by-state score card on health-system performance was issued in 2007 by the Commonwealth Fund, an independent health-quality research group. It graded such factors as overall population health, quality of care, access to care, and avoidable hospitalizations. Of the 13 states with the best scores, 10 have below-average end-of-life costs. And the three states in the Dartmouth study that spend the most on end-of-life health care—New York, New Jersey, and California—ranked 22nd, 26th, and 39th, respectively, in the Commonwealth Fund overall ranking.
A February 2008 study by the nonpartisan Congressional Budget Office found a reverse correlation between per capita Medicare spending and care quality. The percentage of patients hospitalized with heart attacks, pneumonia, and heart failure who get recommended treatments is lower in the higher-spending areas.
"We see huge regional differences in health-care quality," says IBM's Grundy, whose department buys health insurance for 386,000 employees around the world. "There's almost an inverse relationship between cost and quality, with the better quality in the states with a high concentration of primary-care providers," he says.
Primary-care doctors are trained to manage the "whole person," which can help keep seriously ill people doing well and out of the hospital.
Seeing too many specialists produces "fragmentation," says Donald M. Berwick, M.D., president and CEO of the Institute for Healthcare Improvement, a not-for-profit organization based in Cambridge, Mass. "If you have 18 doctors, you'll have more coordination problems than if you have three."
More sensible spending on tests and treatments could take a big bite, perhaps as much as 20 to 30 percent, out of the growing U.S. health-care tab while maintaining or even improving the quality of care, according to the Dartmouth researchers. That savings could help hold down health-care costs for the insured and be used to fund coverage for the tens of millions of Americans who are uninsured or underinsured.
Consumers Union, the nonprofit publisher of Consumer Reports, recommends these policy actions:
Stop rewarding mistakes. Some steps are already being taken. For instance, Medicare will soon stop paying for most treatment of bedsores, hospital infections, and other problems that could be avoided but afflict patients who were originally hospitalized for some other condition. Under current practice, hospitals actually make money from treating their own mistakes.
Encourage primary care. Fewer medical-school graduates are going into primary care because they can make much more money as specialists, no small consideration when faced with paying off six-figure student loans. Medicare is currently studying paying primary-care doctors extra for functioning as a "medical home" for patients, helping to manage their chronic ailments and coordinating care provided by specialists.
Find out what really works. The government should fund more research comparing different treatments for common conditions, and then scale reimbursements to encourage the use of the most effective care. That would help discourage the unnecessary treatments and tests found in high-spending regions.
For people with serious long-term illnesses, navigating America's health-care system can be daunting. Here's what patients and family members can do to increase the chances of getting the best, most humane treatment.
It pays to know what type of care to expect from hospitals in your area. Some are better than others at managing long-term conditions in a way that prevents the need for frequent hospitalizations and specialist visits, and the accompanying risks of infections and medical errors. Check out our free hospital comparison tool to find out where your hospital stands.
What you can do:
Just because a test or treatment can be done doesn't mean it should be done. "Every intervention can create complications," says Donald M. Berwick, M.D., president and CEO of the Institute for Healthcare Improvement, a not-for-profit organization based in Cambridge, Mass.
What you can do:
Having many doctors involved in your care can lead to confusion and miscommunication. "The likelihood of a medication error skyrockets when you receive care from multiple independent practitioners," says Eric A. Coleman, M.D., director of the Care Transitions Program at the University of Colorado Health Sciences Center.
What you can do:
Many errors occur during transfers in the hospital, or to home, a rehab center, or a nursing home. "We reimburse physician care and hospital care, but we don't reimburse care coordination," says Mary Naylor, Ph.D., director of the Center for Transitions and Health at the University of Pennsylvania School of Nursing. "Often primary-care doctors and specialists don't even talk to each other, so the follow-up care after hospitalization may be provided by a physician who doesn't even know the patient was hospitalized."
What you can do:
Families who have lost loved ones after strenuous courses of invasive treatments often say they regret not having recognized sooner that things were going downhill, and adjusting plans and expectations accordingly. "If someone has progressive cancer and is 87, and her kidneys are failing, and doctors recommend ever more treatments for every disease, you need to ask what the larger plan is," says Ira Byock, M.D., director of palliative medicine at Dartmouth-Hitchcock Medical Center in Lebanon, N.H.
What you can do:
More aggressive hospitals more often use treatments such as feeding tubes and cardiopulmonary resuscitation in patients nearing death. But those measures might not extend life for long, if at all, and can be uncomfortable. In regions with aggressive care, "families report more unmet needs and lower satisfaction," says Joan Teno, M.D., professor of community health at Brown University Medical School.
What you can do:
 WASHING MACHINE REVIEWS
WASHING MACHINE REVIEWS GENERATOR REVIEWS
GENERATOR REVIEWS
 Build & Buy Car Buying Service
Build & Buy Car Buying Service
Save thousands off MSRP with upfront dealer pricing information and a transparent car buying experience.
 Get Ratings on the go and compare
Get Ratings on the go and compare
while you shop