Sign In


If you're one of the millions of men and women who suffer from overactive bladder symptoms—the sudden need to urinate, incontinence, making frequent trips to the bathroom—don't be reeled in by recent TV ads that make it seem like drugs are the only solution. The truth is that the drugs are only moderately effective and can trigger side effects so bothersome, such as dry mouth and constipation, that many people quit taking them. Instead, most people can get the relief they need with lifestyle changes, such as cutting back on liquids and caffeine, doing Kegel exercises, and bladder training. Studies have found that behavioral treatments and lifestyle adjustments, when practiced diligently, can help relieve symptoms and can be as effective as medication.

That's why our medical advisers and major medical organizations, such as the American College of Physicians and the American Urological Association (AUA), recommend that you try the nondrug strategies before considering medication.
If following nondrug strategies for several weeks doesn't provide enough relief, it may be time to try adding a medication. If that's the case, you may want to continue the lifestyle changes and behavioral treatments because the two together may be helpful.
For this report, we evaluated the following medications: darifenacin (Enablex); fesoterodine (Toviaz); mirabegron (Myrbetriq); oxybutynin (available as a pill [Ditropan XL and generic], a skin patch [Oxytrol], and a topical gel [Gelnique]); solifenacin (Vesicare); tolterodine (Detrol and generic, Detrol LA and generic); and trospium (generic only).
Our analysis found that none of those drugs are clearly more effective than the others. But they differ in cost and the side effects they cause. Most cause constipation, drowsiness, dry mouth, blurry vision, and dizziness. Myrbetriq works by a different mechanism than the other drugs, so it doesn't cause those side effects, but it can raise blood pressure and increase the risk of urinary tract infections and colds.
Considering the limited effectiveness of overactive bladder medications, and the risk and likelihood of experiencing side effects, we have not chosen a drug as a Consumer Reports Best Buy Drug.
However, if after trying lifestyle changes, you and your doctor conclude that a drug is worth trying, you could consider generic extended-release oxybutynin.
This medicine costs about twice as much as generic short-acting oxybutynin if you are paying out of pocket, but it offers the convenience of once-a-day dosing and research suggests it has a lower risk of side effects than short-acting oxybutynin and some other drugs, including short-acting tolterodine.
Some people tolerate the side effects of generic short-acting oxybutynin tablets well. So if your insurance does not cover medications, you might consider trying that first as it is significantly less expensive.

The hallmark symptom of overactive bladder is a sudden need to urinate. But people with the condition can also leak urine (incontinence) or experience the need to go to the bathroom many times each day—more than eight times—or twice or more while sleeping each night.
The cause of overactive bladder isn't fully understood. In some people, the bladder muscles contract at the wrong time, making it feel like you urgently need to go to the bathroom, or trigger urine leakage. Drugs used to treat the condition relax the bladder muscles, which can increase the storage size of the bladder and reduce the urge to urinate.
The symptoms of overactive bladder are very common. Between 11 and 16 million women in the U.S. experience overactive bladder, according to the federal Agency for Healthcare Research and Quality. Some estimates indicate that an equal number of men also experience overactive bladder, although these symptoms can sometimes be caused by prostate problems.
The condition can develop in men or women of any age, but is more likely to occur in older adults. It's important to note that overactive bladder symptoms are not always that troublesome or permanent and may go away. Studies show that it resolves after a year in for about 35 percent of women who develop it. But for the majority of women, the condition persists for years.
■ Urinating eight or more times per day
■ Waking up more than twice a night to go to the bathroom
■ An overwhelming and sudden need to urinate, even if you've recently gone to the bathroom
■ Leaking urine before you're able to make it to a bathroom. (About half of the people with overactive bladder have urge-related leakage.)
Urgency, incontinence, and urinary frequency can all be caused by having urinary tract infections (UTI), kidney stones, prostate infection or enlargement, or could be from medicine you take to treat other conditions, such as high blood pressure. The first question your doctor might ask if you're having urinary problems is what medicines you're taking. If they don't ask, be sure to bring it up.
Other conditions can cause symptoms similar to those of overactive bladder, too—especially the need to make frequent bathroom trips. These include bladder cancer, diabetes, heart disease, and neurologic disorders, such as multiple sclerosis, Parkinson's disease, spinal cord injuries, and strokes.
Other conditions can also cause urine leakage. For example, "stress incontinence"—leaking urine when you cough, sneeze, run, jump, or even laugh—is sometimes confused with overactive bladder. It's caused by a weakness of the muscles that help keep the bladder closed. Some people have a combination of overactive bladder and stress incontinence.
Another bladder disorder called "overflow incontinence" can have symptoms similar to overactive bladder. This condition is usually caused by an inability to empty the bladder, due to an obstruction or a problem with the muscles that contract the bladder. So much urine builds up in the bladder that it starts leaking out.

Though not life-threatening, overactive bladder is inconvenient, can be embarrassing, and can reduce your quality of life. Some people with the condition find it difficult to leave the house, sit through a meeting, enjoy a dinner out, or go to a movie.
Many people hesitate to seek treatment because they are embarrassed, or because they mistakenly think their symptoms are a normal part of aging and can't be helped. In fact, overactive bladder is not normal, and treatment can ease your symptoms and improve your quality of life.
Your doctor will start by asking about your symptoms and medical history, such as any medications you are taking and any operations or procedures you have undergone. Your doctor might ask you to fill out a "bladder diary" to keep track of how often you go to the bathroom and how often you have urine leakage. Your doctor should also give you a physical examination and check for problems with your urine or bladder.
Most people with overactive bladder can get the relief they need with lifestyle changes, such as cutting back on caffeinated beverages and drinking less fluid between dinner and bedtime, doing Kegel exercises, and bladder training. Studies have found that those nondrug strategies can help relieve symptoms and can be just as effective as medication alone by decreasing the number of trips to the bathroom and how many incontinence episodes you experience.
It's not clear how long the benefits last, but some evidence suggests that many people are helped by bladder training and Kegel exercises for as long as 3 years, but it's difficult to know for certain because those studies have been small. But nondrug measures don't carry the risk of side effects that medications pose.

That's why our medical advisers and major medical organizations, such as the American College of Physicians and the American Urological Association, recommend that you try the nondrug strategies before considering medication.
By reducing the amount of liquids and certain beverages you consume, you can reduce the number of trips you need to make to the bathroom, which might also help reduce leakage episodes as well.
Kegel exercises help by strengthening the pelvic muscles that control urination. And bladder training helps improve bladder control. For example, you might establish a schedule to urinate at regular intervals or hold your urine for progressively longer periods of time. It may take several weeks before you notice a benefit; experts recommend trying bladder training for up to 6 weeks and Kegels for at least 15 weeks.
For more information on those nondrug strategies, see the National Institutes of Health website on overactive bladder.
Find out how to do Kegel exercises correctly
If bladder training, Kegel exercises, and lifestyle adjustments don't provide enough relief, you and your doctor may consider adding a medication. The medicines we evaluated in this report are listed below.
All of these have been approved by the Food and Drug Administration to treat overactive bladder. The oldest are oxybutynin, available since 1976, and tolterodine (Detrol), first approved in 1998. Most of the medications are now available as less expensive generics.
Drugs evaluated in this analysis:
| Generic Name | Brand Name(s) | Available as a Generic Drug? |
| Darifenacin tablet | Enablex | Yes |
| Fesoterodine tablet | Toviaz | Tentative approval |
Mirabegron tablet |
Myrbetriq |
No |
| Oxybutynin tablet | Ditropan XL | Yes |
| Oxybutynin skin gel | Gelnique | No |
| Oxybutynin skin patch | Oxytrol, Oxytrol for Women (OTC) | No |
| Solifenacin tablet | Vesicare | Yes |
| Tolterodine tablet | Detrol, Detrol LA | Yes |
| Trospium tablet | Generic only | Yes |
However, the benefits of overactive bladder medicines can often be marginal and the side effects can cause many people to stop taking them—including blurred vision, constipation, dizziness, dry mouth, and even mental confusion, especially in older people. Because of this, our medical advisers recommend that you try nondrug measures—such as bladder training, Kegel exercises, and the various lifestyle modifications mentioned earlier—before you try a medication. If they don't work, it might be worth trying one of the drugs we discuss. The response to these drugs varies; you might tolerate it well and be able to adapt to the side effects. But you should discuss with your doctor any side effects you experience.
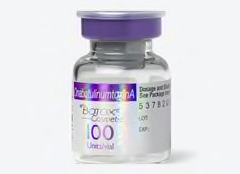
Although clinical trials showed that Botox injections improved overactive bladder symptoms, our medical experts urge caution: the possible side effects can include painful urination, incomplete emptying of the bladder (which could require the insertion of a catheter), and urinary tract infections. The FDA says you should take an antibiotic along with the shot to reduce the risk of developing a UTI.
Moreover, Botox is only approved for use in people who can't take or haven't gotten relief from other overactive bladder medications, and it can be expensive. A single treatment can cost more than $800 without insurance and might need to be repeated every 3 to 8 months.
The overactive bladder drugs are only moderately effective. Studies have found that just a small proportion of people get complete relief from symptoms while taking the medications, particularly over longer periods of time. But most people can expect some relief—a decrease in the number of times a day they feel a strong urge to urinate, and a decline in the number of leakage episodes.
On average, people with overactive bladder urinate 12 times a day. Medication can reduce the number of daily bathroom trips by two to three for most people. If you have incontinence, you can expect the number of episodes to decline by one to two per day.
Of course, people respond differently to the overactive bladder drugs, so there can be variation in the reduction of urges, urinary frequency, and leakage. Some people will notice a substantial decrease in symptoms while others will barely get any relief. The only way to know how you will respond is to try one of the medicines. Also keep in mind that you might have to take the medicine for up to four weeks to see the maximum level of symptom relief.
Each of the seven drugs has strengths and weaknesses. With a few exceptions, studies that have compared the drugs with each other have found little difference among them in terms of effectiveness. That includes studies that compared the immediate-release (or short-acting) forms of these drugs to the long-acting, or extended-release forms. However, the long-acting formulations tend to have fewer side effects such as dry mouth when compared to the short-acting forms, but just as many people stop taking the long-acting forms.

Few studies have evaluated how the drugs affect the highly subjective symptom of urgency. As you might imagine, that's more difficult to measure than the number of times you urinate. Here, too, the studies point to a modest success for the overactive bladder drugs, with a wide range of individual responses. So, depending on your own body chemistry and response, you might notice a meaningful decrease in urgency or very little change.
Overall, more than half of the patients taking an overactive bladder drug stop within six months. Some studies have found that only 10 to 20 percent of people are still taking an overactive bladder medicine after six to 12 months.
That is a very high level of treatment dropout. Some of it is for a good reason: lifestyle changes and nondrug measures have been successful at reducing their symptoms, so the drug is no longer needed. Some dropout may be due to cost, especially for people taking the newer, more expensive drugs. But about a third to one-half of the dropout is due to side effects. Patients simply can't tolerate the drug or decide it's not worth the minimal benefit they get.
Choosing the right overactive bladder drug for you will depend on your medical history, the severity of your condition, convenience factors (such as taking one pill a day vs. two or three times a day), a drug's side effects, your insurance coverage, and your out-of-pocket costs. It will also depend on the other prescription and nonprescription drugs you are taking.
Since older people are more likely to have overactive bladder, doctors are especially alert to any mental confusion they might experience. If you (or someone you care for) has Alzheimer's disease or another form of dementia (for example, dementia that develops after a stroke), your doctor might be reluctant to prescribe a drug for overactive bladder. We'd go a step further and suggest that you not take one unless your doctor feels strongly about prescribing it.
Your doctor will want to know if you have "narrow angle" glaucoma, an eye condition. The overactive bladder medicines are not recommended for people with this type of glaucoma because they can harm their vision—this does not apply to mirabegron (Myrbetriq). But most people with glaucoma have what is called "open angle" glaucoma and can safely take overactive bladder drugs.
| Generic name | Brand Name | Strengths | Weaknesses |
| Darifenacin | Enablex |
|
|
| Fesoterodine | Toviaz |
|
|
Mirabegron |
Myrbetriq |
|
|
| Oxybutynin tablet (Short-acting) | Generic only |
|
|
| Oxybutynin tablet (Extended-release) | Ditropan XL |
|
|
| Oxybutynin transdermal patch | Oxytrol |
|
|
| Oxybutynin topical gel | Gelnique |
|
|
| Solifenacin | Vesicare |
|
|
| Tolterodine (Short-acting) | Detrol |
|
|
| Tolterodine (Extended-release) | Detrol LA |
|
|
Trospium (Short-acting) |
Generic only |
|
|
| Trospium (Extended-release) | Generic only |
|
|

If diligently following nondrug strategies for several weeks doesn't provide enough relief, it may be time to try adding a medication. But if you do decide to try a medication, continue the lifestyle changes and behavioral treatments because studies suggest the combination of a drug and nondrug strategies is more effective than either alone.
If you and your doctor conclude that a medication is worth trying you could consider generic extended-release oxybutynin.
This medicine costs about twice as much as generic short-acting oxybutynin if you are paying out of pocket. But it offers the convenience of once-a-day dosing—that could be a significant advantage for some people, such as seniors, who take multiple medicines per day—and research suggests it has a lower risk of side effects than short-acting oxybutynin and some other drugs, including short-acting tolterodine.
The short- and long-acting forms of generic tolterodine might also be good options because they have a low risk of side effects, and the long-acting form offers once-a-day convenience.
If cost is a major issue for you—for example, if you are without health insurance—we suggest that you talk with your doctor about trying low-cost generic oxybutynin first. Although it has a high rate of adverse effects, some people tolerate it well and it is the least expensive overactive bladder medication, you can find it for as little as $4 for a month's supply at several major retailers like Kroger, Sam's Club, or Walmart. Some stores, such as CVS and Walgreens, require a membership fee to participate and might charge higher prices. There might be other restrictions too, so check the details carefully to make sure your drug and dose are covered.
But if it does not provide you with enough symptom relief or the side effects are bothersome, you might have to try one of the other medicines.

Our evaluation is primarily based on an independent scientific review of the evidence on the effectiveness, safety, and side effects of overactive bladder medications. A team of physicians and researchers at the Pacific Northwest Evidence-Based Practice Center (EPC) conducted the analysis.
A synopsis of that forms the basis for this report. A consultant to Consumer Reports Best Buy Drugs is also a member of the Pacific Northwest EPC research team, which has no financial interest in any pharmaceutical company or product. The full Pacific Northwest EPC review of overactive bladder drugs is available here. (This is a long and technical document written for physicians). We also relied on research conducted by the Agency for Healthcare Research and Quality and the Cochrane Collaboration.
Abrams P., et al., Combination treatment with mirabegron and solifenacin in patients with overactive bladder: Efficacy and safety results from a randomized, double-blind, dose-ranging, phase 2 study (Symphony).European Urology, 2014;67:577-588.
Abrams P, Cardozo L, Fall M, et al. The standardisation of terminology in lower urinary tract function: report from the standardisation subcommittee of the International Continence Society. Urology. 2003;61(1):37-49.
Abrams, P., et al., Tolterodine, a new antimuscarinic agent: as effective but better tolerated than oxybutynin in patients with an overactive bladder. British Journal of Urology, 1998. 81(6): p. 801-10.
Anderson, R.U., et al. Effectiveness and tolerability of extended release oxybutynin vs. extended-release tolterodine in women with or without prior anticholinergic treatment for overactive bladder. International Urogynecology Journal, 2006. 17(5): p. 502-11.
Anderson, R.U., et al. Once daily controlled vs. Immediate release oxybutynin chloride for urge urinary incontinence. Journal of Urology, 1999. 161(6): p. 1809-1812.
Anonymous. Detrol LA package insert. 2002.
Anonymous. Ditropan XL package insert. 2004.
Anonymous. Myrbetriq package insert. 2015.
Anonymous. Trospium chloride (Sanctura): another anticholinergic for overactive bladder. Medical Letter on Drugs & Therapeutics. 2004;46(1188):63-64.
Appell, R.A., et al. Prospective randomized controlled trial of extended-release oxybutynin chloride and tolterodine tartrate in the treatment of overactive bladder: results of the OBJECT Study. Mayo Clinic Proceedings, 2001. 76(4): p. 358-63.
Armstrong, R.B., K.M. Luber, and K.M. Peters, Comparison of dry mouth in women treated with extended-release formulations of oxybutynin or tolterodine for overactive bladder. International Urology & Nephrology, 2005. 37(2): p. 247-52.
Barkin, J., et al. A randomized, double-blind, parallel-group comparison of controlled- and immediate-release oxybutynin chloride in urge urinary incontinence. Clinical Therapeutics, 2004. 26(7): p. 1026-36.
Batista, E. et al., The efficacy and safety of mirabegron compared with solifenacin in overactive bladder patients dissatisfied with previous antimuscarinic treatment due to lace of efficacy: results of a noninferiority, randomized, phase IIIb trial. Therapeutic Advances in Urology, 2015;7(4):167-179.
Beers MH, Ouslander JG, Rollingher I, Reuben DB, Brooks J, Beck JC. Explicit criteria for determining inappropriate medication use in nursing-home residents. Arch Intern Med. 1991;151(9):1825-1832.
Beers MH. Explicit criteria for determinig potentially inappropriate medication use by the elderly. An update. Arch Intern Med. 1997;157(4):1531-1537.
Birns, J., et al. A randomized controlled trial comparing the efficacy of controlled-release oxybutynin tablets (10 mg once daily) with conventional oxybutynin tablets (5 mg twice daily) in patients whose symptoms were stabilized on 5 mg twice daily of oxybutynin. BJU International, 2000. 85(7): p. 793-798.
Burgio KL, Locher JL, Goode PS, et al. Behavioral vs drug treatment for urge urinary incontinence in older women. JAMA. 1998; 280:1995-2000.
Chapple, C.R., et al., Clinical efficacy, safety, and tolerability of once-daily fesoterodine in subjects with overactive bladder. European Urology, 2007. 52:1204-1212.
Chapple, C.R. and P. Abrams, Comparison of darifenacin and oxybutynin in patients with overactive bladder: assessment of ambulatory urodynamics and impact on salivary flow. European Urology, 2005. 48(1): p. 102-9.
Chapple, C.R., et al. A comparison of the efficacy and tolerability of solifenacin succinate and extended-release tolterodine at treating overactive bladder syndrome: Results of the STAR trial. European Urology, 2005. 48(3): p. 464-70.
Chapple, C.R., et., A phase II dose-ranging study of mirabegron in patients with overactive bladder. International Urogynecology Journal. 2013. 24:1447-1458.
Chapple, C.R., et al., Randomized double-blind, active-controlled phase 3 study to assess 12-month safety and efficacy of mirabegron, a β3-adrenoceptor agonist, in overactive bladder. European Urology, 2013, 63:296-305.
Chapple, C.R., et al., Randomized, double-blind placebo- and tolterodine-controlled trial of the once-daily antimuscarinic agent solifenacin in patients with symptomatic overactive bladder. BJU International, 2004. 93:303-310.
Chapple, C.R., et al., Solifenacin appears effective and well tolerated in patients with symptomatic idiopathic detrusor overactivity in a placebo- and tolterodine-controlled phase 2 dose-finding study. BJU International, 2004. 93:71-77.
Chapple, C.R., et al. Treatment outcomes in the STAR study: a subanalysis of solifenacin 5 mg and tolterodine ER 4 mg. European Urology, 2007. 52(4): p. 1195-203.
Choo, M.-S., et al., Efficacy and safety of solifenacin succinate in Korean patients with overactive bladder: A randomized, prospective, double-blind, multicenter study. International Journal of Clinical Practice, 2008. 1675-1683.
Chu, F.M., et al. Extended-release formulations of oxybutynin and tolterodine exhibit similar central nervous system tolerability profiles: a subanalysis of data from the OPERA trial. American Journal of Obstetrics & Gynecology, 2005. 192(6): p. 1849-54.
Couture JA, Valiquette L. Urinary incontinence. Ann Pharmacother. 2000;34(5):646-655.
Davila, G.W., C.A. Daugherty, and S.W. Sanders. A short-term, multicenter, randomized double-blind dose titration study of the efficacy and anticholinergic side effects of transdermal compared to immediate release oral oxybutynin treatment of patients with urge urinary incontinence. Journal of Urology, 2001. 166(1): p. 140-145.
Diokno, A.C., et al. Prospective, randomized, double-blind study of the efficacy and tolerability of the extended-release formulations of oxybutynin and tolterodine for overactive bladder: Results of the OPERA trial. Mayo Clinic Proceedings, 2003. 78(6): p. 687-695.
Dmochowski, R.R., et al. Comparative efficacy and safety of transdermal oxybutynin and oral tolterodine vs. placebo in previously treated patients with urge and mixed urinary incontinence. Urology, 2003. 62(2): p. 237-42.
Dmochowski, R.R., et al. Randomized, double-blind study of controlled-release Oxybutynin and Tolterodine for overactive bladder (Abstract). Proceedings of the International Continence Society, 2001.
Drutz, H.P., et al. Clinical efficacy and safety of tolterodine compared to oxybutynin and placebo in patients with overactive bladder. International Urogynecology Journal, 1999. 10(5): p. 283-9.
Ercan O., et al., Comparison of solifenacin and fesoterodine in treatment of overactive bladder. Saudi Medical Journal, 2015. 36(10):1181-1185.
Fantl JA, Newman DK, Colling J, et al. Urinary incontinence in adults: acute and chronic management. Clinical Practice Guideline #2 AHCPR Publication No. 96-0682. Rockville, MD: Agency for Healthcare Policy and Research; 1996.
Garnett S, Abrams P. The natural history of the overactive bladder and detrusor overactivity. A review of the evidence regarding the long-term outcome of the overactive bladder. J Urol. 2003;169(3):843-848.
Halaska, M., et al. Controlled, double-blind, multicentre clinical trial to investigate long-term tolerability and efficacy of trospium chloride in patients with detrusor instability. World Journal of Urology, 2003. 20(6): p. 392-9.
Herschorn, S., et al. Comparison of fesoterodine and tolterodine extended release for the treatment of overactive bladder: A head-to-head placebo-controlled trial. BJU International, 2009. 105:58-66.
Herschorn, S. et al., Tolerability of 5 mg solifenacin once daily versus 5 mg oxybutynin immediate release 3 times daily: Results of the VECTOR trial. Journal of Urology, 2010. 183:1892-1898
Ho, C-H., et al., Solifenacin and tolterodine are equally effective in the treatment of overactive bladder symptoms. Journal of Formos Med Assoc, 2010. 109(10):702-708.
Homma, Y. and K. Kawabe. Health-related quality of life of Japanese patients with overactive bladder treated with extended-release tolterodine or immediate-release oxybutynin: a randomized, placebo-controlled trial. World Journal of Urology, 2004. 22(4): p. 251-6.
Homma, Y., et al. Clinical efficacy and safety of tolterodine extended-release for treatment of overactive bladder. A phase II, 12-week, randomised, double-blind, placebo- and active (oxybutynin)-controlled study in Japan and Korea (Abstract). Proceedings of the International Continence Society, 2002.
Homma, Y., et al. Clinical efficacy and tolerability of extendedrelease tolterodine and immediate-release oxybutynin in Japanese and Korean patients with an overactive bladder: a randomized, placebo-controlled trial. BJU International, 2003. 92(7): p. 741-7.
Hsiao, S.-M., et al., Comparison of urodynamic effects, therapeutic efficacy and safety of solifenacin versus tolterodine for female overactive bladder syndrome. Journal of Obstrectics and Gynaecological Research, 2011. 37(8):1084-1091.
Kaplan, S.A., et al., Superior efficacy of fesoterodine over tolterodine extended release with rapid onset: A prospective, head-to-head, placebo-controlled trial. BJU International, 2010. 107:1432-1440.
Kessler, T.M., et al., Adverse event assessment of antimuscarinics for treating overactive bladder: A network meta-analytic approach. PLoS ONE, 2011. 6(2):e16718.
Koda-Kimble, et al., eds. Applied therapeutics: the clinical use of drugs, 7th ed. Baltimore, MD: Lippincott Williams & Wilkins; 2001.
Kosilov, K., et al., A randomized, controlled trial of effectiveness and safety of management of OAB sysptoms in elderly men and women with standard-dosed combination of solifenacin and mirabegron. Archives of Gerontology and Geriatrics, 2015. 61:212-216.
Khullar, V., et al., Efficacy and tolerability of mirabegron, a β3-adrenoceptor agonist, in patients with overactive bladder: Results from a randomized European-Australian phase 3 trial. European Urology, 2013. 63:283-295.
Kuo, H-C., et al., Results of a randomized, double-blind, parallel-group, placebo- and active-controlled, multicenter study of mirabegron a β3-adrenoceptor agonist, in patients with overactive bladder in Asia. Neurology and Urodynamics, 2015. 34:685-692.
Lee, J.G., et al., Tolterodine: As effective but better tolerated than oxybutynin in Asian patients with symptoms of overactive bladder. International Journal of Urology, 2002. 9(5): p. 247-252.
Leung, H.Y., et al. A randomized controlled trial of tolterodine and oxybutynin on tolerability and clinical efficacy for treating Chinese women with an overactive bladder. BJU International, 2002. 90: p. 375-380.
Madersbacher, H., et al. Trospium chloride vs. oxybutynin: a randomized, double-blind, multicentre trial in the treatment of detrusor hyper-reflexia. British Journal of Urology, 1995. 75(4): p. 452-6.
Malone-Lee, J., et al. The comparative tolerability and efficacy of tolterodine 2 mg bid vs. oxybutynin 2.5/5 mg bid in the treatment of the overactive bladder. Neurourology & Urodynamics, 1998. 17(4): p. 163-164.
Malone-Lee, J., et al. Tolterodine: superior tolerability than and comparable efficacy to oxybutynin in individuals 50 years old or older with overactive bladder: a randomized controlled trial. Journal of Urology, 2001. 165(5): p. 1452-6.
Maman, K., et al., Comparative efficacy and safety of medical treatments for the management of overactive bladder: A systematic literagure review and mixed treatment comparison. European Urology, 2014. 65:755-765.
McEvoy, et al., eds. AHFS Drug Information 2002. Bethesda, MD: Society of Health System Pharmacists, Inc.; 2002.
Milani, R., et al. Double-blind crossover comparison of flavoxate and oxybutynin in women affected by urinary-urge syndrome. Int Urogynecol J, 1993. 4(1): p. 3-8.
Nilsson, C.G., et al. Comparison of a 10-mg controlled release oxybutynin tablet with a 5-mg oxybutynin tablet in urge incontinent patients. Neurourology & Urodynamics, 1997. 16(6): p. 533-542.
Radomski, S., et al. Preliminary evaluation of a new controlled release oxybutynin in urinary incontinence. Current Medical Research and Opinion, 2004. 20(2): p. 249-253.
Sand, P.K., et al. A comparison of extended-release oxybutynin and tolterodine for treatment of overactive bladder in women. International Urogynecology Journal, 2004. 15(4): p. 243-8.
Sand, P.K., et al., Randomized, double-blind study to compare extended-release oxybutynin and tolterodine for overactive bladder. Obstetrics & Gynecology, 2001. 97(4): p. S49.
Schmidt RA, Zermann DH, Doggweiler R. Urinary incontinence update: Bold traditions and new concepts. Adv Intern Med. 1999;44:19-57.
Sussman, D. and A. Garely. Treatment of overactive bladder with once-daily extended-release tolterodine or oxybutynin: The Antimuscarinic Clinical Effectiveness Trial (ACET). Current Medical Research & Opinion, 2002. 18(4): p. 177-184.
Swift, S., et al. A new once-daily formulation of tolterodine provides superior efficacy and is well tolerated in women with overactive bladder. International Urogynecology Journal, 2003. 14(1): p. 50-4; discussion 54-5.
Van Kerrebroeck, P., et al. Tolterodine once-daily: superior efficacy and tolerability in the treatment of the overactive bladder. Urology, 2001. 57(3): p. 414-21.
Van Kerrebroeck, P.E., G. Serment, and E. Dreher. Clinical efficacy and safety of tolterodine compared to oxybutynin in patients with overactive bladder [abstract]. Neurourology & Urodynamics, 1997. 16(5): p. 478-479.
Versi, E., et al. Dry mouth with conventional and controlledrelease oxybutynin in urinary incontinence. Obstetrics & Gynecology, 2000. 95(5): p. 718-721.
Yamaguchi, O. et al., Phase III, randomized, double-blind, placebo-controlled study of the β3-adrenoceptor agonist mirabegron, 50 mg once daily, in Japanese patients with overactive bladder. BJU International. 2014, 113:951-960.
Zeegers, A.G.M., et al. Conservative therapy of frequency, urgency, and urge incontinence: A double-blind clinical trial of flavoxate hydrochloride, oxybutinin chloride, emepronium bromide, and placebo. World Journal of Urology, 1987. 5(1): p. 57-61.
Zellner, M., et al., Trospium chloride and oxybutynin hydrochloride in a German study of adults with urinary urge incontinence: Results of a 12-week, multicenter, randomized, double-blind, parallel-group, flexible-dose noninferiority trial. Clinical Therapeutics, 2009. 31(11):2519-2539.
Zinner, N., J. Tuttle, and L. Marks. Efficacy and tolerability of darifenacin, a muscarinic M3 selective receptor antagonist (M3 SRA), compared with oxybutynin in the treatment of patients with overactive bladder. World Journal of Urology, 2005. 23(4): p. 248-52.
These materials are made possible by a grant from the state Attorney General Consumer and Prescriber Education Grant Program, which is funded by the multi-state settlement of consumer-fraud claims regarding the marketing of the prescription drug Neurontin (gabapentin).
 Build & Buy Car Buying Service
Build & Buy Car Buying Service
Save thousands off MSRP with upfront dealer pricing information and a transparent car buying experience.
 Get Ratings on the go and compare
Get Ratings on the go and compare
while you shop